Me & My Fat – The Role of Fat on Your Hormonal Health

Fat, a word dreaded by many depending on the context. In adequate amounts, it’s beneficial to our health when both consumed, or stored. But too little or too much can have severely negative health outcomes. Obesity and being overweight were once seen as being both positive and attractive; only the wealthy could afford to eat! As the world progressed past the industrial era, more were able to afford food. Enter the 21st century where high calorie processed westernised diets are rampant around the world, now affordable by many. Jobs in the west and increasingly so in the rest of the world are switching from active to sedentary desk-based work, too. The concurrent increase in sedentary lifestyles and easily accessible and affordable high calorie diets has led to a boom in the number of overweight and obese people in the world. The modern world has known for some time now about the detrimental health effects that excess adipose tissue can place on our health too. It may be arguably more detrimental than too little fat (not to be desired, either!). However, both are diseases that have detrimental effects on our overall health, especially our hormonal health. So, let’s dive deeper into the role of your fat on your health, with a focus on your hormonal health.
Adipose Tissue & The HPG Axis
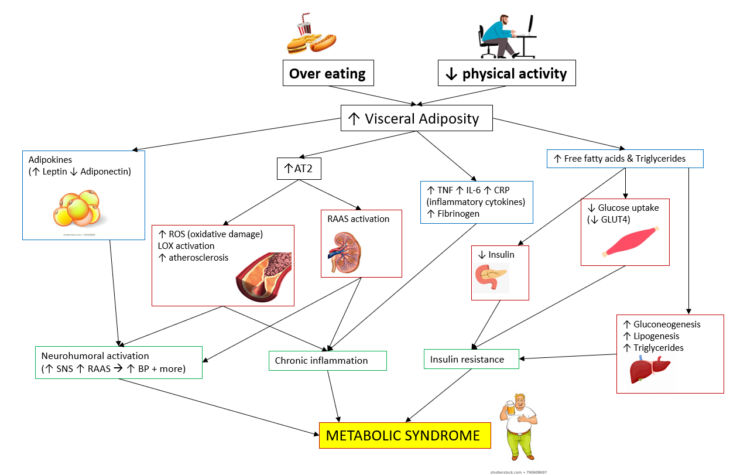
It shouldn’t be surprising to hear that clinical obesity and being overweight are frequently associated with hypogonadism. In-fact, low testosterone is considered a ‘hallmark’ of metabolic syndrome in men 1. If you’re unaware of metabolic syndrome, it’s a cluster of diseased conditions which occur together. They increase your risk of proinflammatory state, mental health disorders, fatigue, atherosclerotic plaque build-up (increased risk of stroke), other cardiovascular heart diseases, and type 2 diabetes mellitus. It often sees increased blood pressure, high blood sugar, excessive abdominal fat, abnormal cholesterol and/or triglyceride levels, and low testosterone in men.
To explain metabolic syndrome a bit better, I’ve drawn a diagram describing the pathophysiological mechanisms that are involved in metabolic syndrome 2. There will be bits you will not be familiar with and so these are described below:
- AT2 is angiotensin II receptor 2 – Involved in the renin-angiotensin system (RAS).
- Adipokines – Cell signalling proteins secreted by adipose tissue (fat), which control inflammation, appetite, insulin sensitivity, and fat cell growth.
- TNF, IL-6, & CRP – All inflammatory cytokines that promote inflammation. GLUT4 is the glucose transporter for glucose in skeletal muscle (ie. your biceps)
- Gluconeogenesis – A metabolic pathway that produces glucose from non-carbohydrate sources, occurring primarily in the liver.
- Lipogenesis – As you’ve probably guessed, it’s the metabolic formation of fats, which gets stored in the fat cell of adipose tissue!
- Fibrinogen – Made in the liver and is involved in clotting (when converted to fibrin by thrombin), too much and you risk thrombosis and vascular injuries.
- Visceral fat – The hormonally active component of body fat, which is normally packed between organs. It’s mostly found around the abdomen, giving rise to the classic beer belly look. It’s also the most dangerous type of fat for your health, when carried in excess.
Metabolic syndrome is primarily a by-product of over eating, excess alcohol, and a decrease in physical activity, though genetics play a role, where Hispanics and Asians have a higher risk for metabolic syndrome than other ethnicities 3.
Let’s move back specifically to the HPG Axis (HPGA). Adipose tissue controls critical metabolic functions, including food intake, insulin sensitivity, vascular reactivity, and immunity. Likewise, testosterone and oestradiol will deeply affect fat mass distribution and size 1. Before I describe the relationship of fat with the HPGA, you need to know it’s a complex interaction. Anything that is related to the metabolic and endocrinological systems will be complex and intertwined; you must appreciate the intrinsic beauty in this complexity. Life and its many organisms have never been simple.
Leptin & Testicular Function
Did you pay attention? You noticed that fat cells produce the adipokine are called ‘leptin’, right? As adipose tissue increases in size and fat cell density, leptin production increases. So, the more fat you accrue, the more leptin you make. This is especially true with visceral fat. Leptin is an adipokine, that is a cytokine-like hormone. It’s involved in the regulation of energy homeostasis (normal function), neuroendocrine function (brain-hormone) with particular effects on appetite (acts to suppress it), immunity, lipid and glucose homeostasis, and fatty acid oxidation 4,5. So what?
Well, it seems that excess leptin has a negative impact on Leydig cell function. In cultured rat Leydig cells, leptin in excess will strongly inhibit hCG stimulated testosterone production in a dose-dependent manner. We see this this effect occurring at concentrations too, in obese men. Additionally, leptin is known to regulate the gonadotropic, thyrotrophic, and adrenal axes 6.
Okay, you are not a rat and correlation does not equal causation, right? The relationship may be non-linked; obese men have lower Testosterone regardless, does that mean leptin decreases it? It’s hard to say – there is a lack of clinical data. But leptin regulates and promotes several other important functions, all of which certainly can affect your Testosterone and HPGA.
With an increase in leptin, we may see leptin resistance develop in the brain and in other tissues 7. Much like how insulin resistance develops. Normally, leptin would decrease insulin secretion and appetite. Unfortunately, we are in a situation now where we see increased insulin secretion and appetite due to leptin resistance. Resultingly, we are at risk of type 2 diabetes mellitus. Insulin is normally capable of stimulating testosterone production 8, but with increased insulin resistance, we may begin to see a decrease in testosterone production. Is this the primary cause of lowered testosterone we see with gaining excess fat? No, it’s a contributing factor, one among many.
The Double A Team: Adipose & Aromatase
We also know that adipose tissue is a rich source of aromatase enzyme; aromatase expression (production of the enzyme) in adipose tissue primarily accounts for the peripheral formation of oestrogen, respectively increasing as body fat increases 9. With increased conversion of Testosterone to Oestradiol, we see a decrease in GnRH secretion, further decreasing testosterone levels, which in turn further increases deposition of fat within the abdominal and visceral fat, further encouraging greater oestrogen production, a ‘hypogonadal-obesity cycle’, if you’d like 1,10–12.
Let’s remind ourselves of the Hypothalamic-pituitary-testicular axis (HPTA) and how it works, best described by a picture sourced from asih (click for full-sized image):
Of course, this is also missing DHT, and inhibin, but let’s ignore that for now as oestradiol is the most important thing to note here. Oestradiol is a strong inhibitor of GnRH production and gonadotropin secretion. So, it’s understandable that an increase in oestradiol will reduce testosterone production, but when there’s excess body fat, we’re in a situation where the cycle worsens and worsens as with hypogonadism, we are at an increased risk of excess body fat gain, only encouraging the problem further.
Sweet Dreams, Or Tiring & Constant Awakenings? Excess Adipose Tissue & Obstructive Sleep Apnoea
We come back to a chicken or egg question, again – what came first? This time, we question if it is the excess weight gain, or obstructive sleep apnoea (OSA)? OSA can occur independent of excess weight and then predispose a person to excess weight gain, due to sleep deprivation, daytime sleeping, and disrupted metabolism . OSA is also associated with increase sympathetic nervous activation, sleep fragmentations, poor quality sleep, all of which increases insulin resistance, potentially leading to type 2 diabetes mellitus, and helping further facilitate a path to obesity. We also see alterations in leptin, ghrelin, and orexin; all involved in appetite control, and an increase in appetite will likely lead to an increase in fat gain, unless you will yourself to control your food intake. But it can often be quite hard to ignore the pain of a hungry stomach and the constant replay of food and cravings in your head. We then see a vicious cycle where obesity and OSA worsen each other 13.
Sleep disorders in general already negatively affect testosterone production; you’ll know this if you followed my blog on the endocrine system and sleep. A normal and healthy circadian rhythm is extremely important to ensure adequate testosterone production and good health. Therefore, it comes at little surprise that OSA can cause low testosterone and elevated oestradiol. We also know that large doses of exogenous testosterone and anabolic/androgen steroid abuse are associated with abnormalities of sleep duration and composition, which can further worsen general health and raise oestradiol, not an ideal situation.
Adipose Tissue & General Health
What we need is adequate adipose tissue. As I’ve mentioned, fat is an endocrine hormone that regulates your metabolism and therefore has a knock-on effect on many processes, even your mental health. But in excess, we will run into issue. All the same, too little and health issues become apparent. Let’s explore the two a bit…
Not Enough Fat
- Generally associated with chronic illness and starvation
- Among bodybuilders who purposely aim for competition bodyfat, there is a decrease in physical performance and a reduction in normal immune system function 14
- We also see a decrease in testosterone concentrations in natural bodybuilders.
- Significantly lowered oestradiol, which also has negative health consequences 14
- Hypogonadism 14
- Lowered thyroid hormone
- Worsened mental health
This is to be expected; we see a decrease in important adipokines which also regulate the immune system, oestradiol, and alteration in metabolism. To note, the case study I refer to saw the bodybuilder go from 14.8% to 4.5% body fat. Generally, ‘normal’ would be considered from the range of 17.6% – 25.3% in men 15. Bear in mind that studies that investigate this can’t account for all aspects of health. We see perfectly healthy individuals who are as low as 8% body fat, but it becomes harder to maintain a normal state of health any lower. So, what’s an ideal healthy body fat range for a man? The answer is: we need more studies.
Too Much Fat
- Cardiometabolic dysfunction 16
- Skeletal muscle dysfunction 17
- Metabolic syndrome
- Impaired immune system and proinflammatory state 18
- Type 2 diabetes mellitus 19
- Worsened mental health 20
- Liver and kidney diseases 21
- Obstructive sleep apnoea 22
- Hypogonadism 23
Conclusion
To conclude, the final message is very clear: follow a healthy lifestyle and eat to your appropriate energy needs with adequate vegetables, fruits, healthy fats (omega 3/6 and PUFA/MUFAs, less saturated and trans fats), protein, fibre, and carbohydrate intake; count your calories, macronutrients and micronutrients, but don’t overeat. Do exercise often, preferably daily, with a mixture of cardiovascular and resistance strength training; aim to improve your fitness and strength too. Likewise, don’t chronically diet to the point where you don’t have adequate body fat either. Aim to be healthy; be optimal, avoid the states of over fat and under fat; be the best you can, and have fun doing it!
References
- Mammi C, Calanchini M, Antelmi A, et al. Androgens and Adipose Tissue in Males: A Complex and Reciprocal Interplay. Int J Endocrinol. 2012;2012:1-8. doi:10.1155/2012/789653
- Rochlani Y, Pothineni NV, Kovelamudi S, Mehta JL. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther Adv Cardiovasc Dis. 2017;11(8):215-225. doi:10.1177/1753944717711379
- Marc J. Genetic Succeptibility to Metabolic Syndrome. EJIFCC. 2007;18(1):7.
- Tilg H, Moschen AR. Adipocytokines: Mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol. 2006;6(10):772-783. doi:10.1038/nri1937
- Ahima RS. Adipose tissue as an endocrine organ. Obesity (Silver Spring). 2006;14 Suppl 5. doi:10.1038/oby.2006.317
- Paz-Filho G, Wong M-L, Licinio J, Mastronardi C. Leptin therapy, insulin sensitivity, and glucose homeostasis. Indian J Endocrinol Metab. 2012;16(9):549. doi:10.4103/2230-8210.105571
- Gruzdeva O, Borodkina D, Uchasova E, Dyleva Y, Barbarash O. Leptin resistance: Underlying mechanisms and diagnosis. Diabetes, Metab Syndr Obes Targets Ther. 2019;12:191-198. doi:10.2147/DMSO.S182406
- Pasquali R, Casimirri F, De Iasio R, et al. Insulin regulates testosterone and sex hormone-binding globulin concentrations in adult normal weight and obese men. J Clin Endocrinol Metab. 1995;80(2):654-658. doi:10.1210/jcem.80.2.7852532
- Nelson LR, Bulun SE. Estrogen production and action. J Am Acad Dermatol. 2001;45(3):S116-S124. doi:10.1067/mjd.2001.117432
- Sharleen Sidhu, Parikh Tanvi BK. Endocrine Changes in Obesity. In: Perioperative Anesthetic Care of the Obese Patient. CRC Press; 2009:41-49. doi:10.3109/9781420095319-6
- Strain GW, Zumoff B, Miller LK, et al. Effect of massive weight loss on hypothalamic Pituitary-Gonadal function in obese men. J Clin Endocrinol Metab. 1988;66(5):1019-1023. doi:10.1210/jcem-66-5-1019
- Bélanger C, Luu-The V, Dupont P, Tchernof A. Adipose tissue intracrinology: Potential importance of local androgen/estrogen metabolism in the regulation of adiposity. Horm Metab Res. 2002;34(11-12):737-745. doi:10.1055/s-2002-38265
- Pillar G, Shehadeh N. Abdominal Fat and Sleep Apnea: The chicken or the egg? Diabetes Care. 2008;31(Supplement 2):S303-S309. doi:10.2337/dc08-s272
- Rossow LM, Fukuda DH, Fahs CA, Loenneke JP, Stout JR. Natural Bodybuilding Competition Preparation and Recovery: A 12-Month Case Study.; 2013. www.IJSPP-Journal.com. Accessed May 29, 2020.
- Branco BHM, Bernuci MP, Marques DC, et al. Proposal of a normative table for body fat percentages of Brazilian young adults through bioimpedanciometry. J Exerc Rehabil. 2018;14(6):974-979. doi:10.12965/jer.1836400.200
- Maffetone PB, Rivera-Dominguez I, Laursen PB. Overfat Adults and Children in Developed Countries: The Public Health Importance of Identifying Excess Body Fat. Front Public Heal. 2017;5. doi:10.3389/fpubh.2017.00190
- Tallis J, James RS, Seebacher F. The effects of obesity on skeletal muscle contractile function. J Exp Biol. 2018;221(13). doi:10.1242/jeb.163840
- de Heredia FP, Gómez-Martínez S, Marcos A. Obesity, inflammation and the immune system. Proc Nutr Soc. 2012;71(2):332-338. doi:10.1017/S0029665112000092
- Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes, Metab Syndr Obes Targets Ther. 2014;7:587-591. doi:10.2147/DMSO.S67400
- Rajan TM, Menon V. Psychiatric disorders and obesity: A review of association studies. J Postgrad Med. 2017;63(3):182-190. doi:10.4103/jpgm.JPGM_712_16
- Ix JH, Sharma K. Mechanisms linking obesity, chronic kidney disease, and fatty liver disease: The roles of fetuin-A, adiponectin, and AMPK. J Am Soc Nephrol. 2010;21(3):406-412. doi:10.1681/ASN.2009080820
- Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK. Interactions between obesity and obstructive sleep apnea: Implications for treatment. Chest. 2010;137(3):711-719. doi:10.1378/chest.09-0360
- de Lorenzo A, Noce A, Moriconi E, et al. MOSH syndrome (Male obesity secondary hypogonadism): Clinical assessment and possible therapeutic approaches. Nutrients. 2018;10(4). doi:10.3390/nu10040474