The Thyroid & The HPG Axis

If you’ve much interest in TRT , then you likely know a bit about the Hypothalamic Pituitary Testicular Axis (HPTA). You’ll know how relatively ‘simple’ it can be; hypothalamus in the brain produces a hormone called Gonadotropin Releasing Hormone (GnRH), which tells the anterior pituitary in the brain to release Luteinizing & follicle stimulating hormones (LH & FSH respectively), which tell the gonads (testes in the case of the HPTA) to make Testosterone (T). Some of that T gets converted into Oestradiol (E2) and some to Dihydrotestosterone (DHT), and some is made in the testes. DHT, T & E2 tell the anterior pituitary to basically reduce the amount of LH & FSH released. It also reduces the production of GnRH in the hypothalamus. The cycle continues. The figure below wonderfully sums this up 1:
The truth is that it gets a little bit more complex than this. There’s also inhibin, activin, leptin (hormone produce by fat tissue), insulin and ghrelin (hunger hormone), and kisspeptin which all play their role in this cycle. Insulin and leptin are stimulatory on the hypothalamus (makes more GnRH), inhibin reduces LH & FSH release, ghrelin is inhibitory on the hypothalamus 2,3 .
One thing that’s very influential and often overlooked in this cycle are thyroid hormones. So, this article will examine it in a bit more detail.
Thyroid Hormones
Thyroid hormones, triiodothyronine (T3) & thyroxine (T4) are based and released by the thyroid gland. Your thyroid gland is a small butterfly shaped gland in your neck, just in front of your windpipe. These hormones serve to primarily regulate your body’s metabolism. Both T3 and T4 are partially made up of iodine. Hence why iodine is important for the production of thyroid hormones. The figure below shows how the thyroid gland appears 4:
I’m sure many of you know that Thyroid hormones are renown for ‘burning fat’, in addition to muscle (when thyroid hormones are in excess). They do much more than this; they are essential for correct growth and development, regulating bone growth, neural (brain) maturation, your sensitivity to catecholamines such as adrenaline (thus regulating stress), affecting protein synthesis, and affecting protein, fat, and carbohydrate metabolism, in addition to stimulating vitamin metabolism.
This is why hypothyroidism can lead to various severe symptoms, including hair loss, fatigue, mood and memory alterations, elevated cholesterol, feeling cold, weight gain, cardiac disorders, constipation, sore muscles and joints, dry skin, depression, and altered fertility (reduced Testosterone, erectile dysfunction, etc). Hyperthyroidism equally carries not so nice symptoms, ranging from rapid heartbeats, bulging eyes, heat intolerance, excessive weight loss, cardiac disorders, diarrhoea, strength loss, and more. Go too high and you can die.
Thyroid hormones do this via binding to thyroid hormone receptors (THR), activating a range of changes inside the cell (in a nutshell, though it’s obviously more complex than this). Keeping your thyroid healthy is clearly important, yet the prevalence of hypothyroidism in the UK is 2% (more common in women by 10x) 5. Hyperthyroidism prevalence in the UK is prevalent in 0.2% of men in the UK.
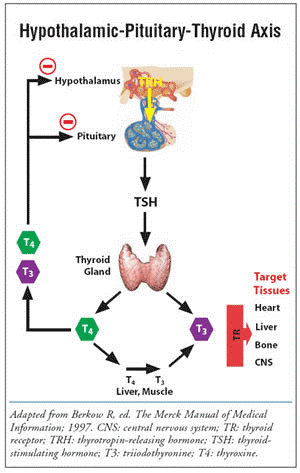
The control of thyroid hormones is established by the Hypothalamic-Pituitary-Thyroid axis (HPT), where the hypothalamus creates a hormone called Thyrotropin-releasing hormone (TRH), stimulating the anterior pituitary gland to release Thyroid-stimulating hormone (TSH), which stimulates the thyroid gland to create and release thyroid hormones. The thyroid hormones negatively feedback to the anterior pituitary gland and hypothalamus, inhibiting TRH & TSH. The cycle continues, going up and down around baseline, much like in the HPTA. The figure below sums up the HPA:
Causes of Hypo/Hyperthyroidism
It’s worth mentioning potential causes of hypo and hyperthyroidism, respectively. In the case of hypothyroidism 6:
- The immune system attacks the thyroid gland, damaging it; Hashimoto’s disease is the most common type of autoimmune reaction which causes this
- Previous thyroid treatment, i.e. due to surgery at the thyroid or radioactive iodine therapy
- A lack of dietary iodine (uncommon in the UK)
- Congenital hypothyroidism (at birth – can be due to various reasons).
- Some viral infections can induce hypothyroidism
- Lithium use
- Amiodarone use (often used to treat irregular heartbeats)
- Interferon treatment (used to treat many cancers and hep C)
In the case of hyperthyroidism7:
- Graves’ diseases, which affects the vast majority of people with hyperthyroidism. This is another autoimmune condition. Smoking can increase the risk of getting it and it often is inherited (gene-related)
- Thyroid nodule development: lumps develop on the thyroid (non-cancerous). Typically affects those >60 years old
- Excess iodine intake
- High levels of human chorionic gonadotrophin (hCG)
- Pituitary adenomas (non-cancerous tumour in the pituitary gland)
- Thyroiditis – this is inflammation of the thyroid
- Thyroid cancer (rare)
Testosterone & Thyroid Hormones – The Relationship
As mentioned, hypothyroidism can decrease Testosterone. It’s well known that primary hypothyroidism (destruction of the thyroid gland, thus indicating the importance of thyroid hormones specifically in preventing hypogonadism) is associated with hypogonadotropic hypogonadism, reversible with thyroid hormone replacement therapy 8 . This was initially thought to be due to hypothyroidism causing lowered Sex Hormone Binding Globulin (SHBG) levels, though we will also note such patients have low free T too; it normalizes when hypothyroidism is treated 9. Note that if you were to reduce SHBG, you’d raise free T and E2, which would ultimately lead to lower Total T, due to the negative feedback loop. But this doesn’t necessarily appear to be the primary cause in hypothyroidism.
T3 may directly modulate LH induced T and E2 production in the Leydig cells, which would make sense given that the testis have THRs and are a prime target for T3 10. This certainly appears to be the case in animal studies, and humans appear to follow the same trend. It also appears that T3 directly increase Leydig cell LH receptor numbers and the mRNA levels of steroidogenic enzymes and regulatory proteins. In a nutshell, that means it directly improves your balls response to LH and helps make more T 11. As to whether this is the exact main cause of action, it’s up for debate.
Conversely, hyperthyroidism is known to increase the concentration of SHBG and Total T, with free T keeping generally normal. However, it’s well associated with erectile dysfunction, decreased libido, and abnormalities of sperm motility 9. The cause of elevated SHBG is likely due to increased liver production of SHBG with elevated T3, given that liver SHBG biosynthesis is regulated by T3 12,13. If you read my article on TRT, SHBG, & Health , you can learn plenty more on the topic. Likewise, you can read about the knock-on effects of low and high SHBG, and therefore the need for control.
The relationship isn’t one way, either. Testosterone, where liver function is normal, is known the significantly release Thyroid Binding Globulin (TBG) when used to treat hypogonadism, indicating that sex-hormone receptors in the liver play a role in stimulating the production of TBG 14. As you can guess from the name, TBG binds to thyroid; its purpose is to transport thyroid hormones. If TBG levels are low, total thyroid levels with be low and free thyroid hormones will be normal or low; an increase in TBG can result in an increase in total thyroid hormones without an increase in free hormone activity in the body.
What Learnings Can We Take From This?
Unfortunately, some “TRT Clinics” not run by medical professionals (i.e. a medical doctor), forget to check for hypothyroidism before embarking you on a lifelong TRT protocol. TRT is a decision for life; it shouldn’t be taken lightly – it comes with complications. Of course, any complications are minimised when dealt with by a well experienced & knowledgeable medical professional, i.e. Dr. Stevens. But it’s still important to check all potential underlying causes of hypogonadism before jumping the gun on treatment and seeing if we can reverse hypogonadism by other means. Once exhausted, TRT becomes an option to consider. I recommend reading my article on How to Increase Testosterone Levels Naturally.
One interesting take is for those with low SHBG. Some patients appear to have low SHBG regardless of protocol. This can be due to genetic causes 15,16. I can attest, I naturally have very low levels of serum SHBG. I also have mutant genes known to be involved with lower SHBG, as establish by my 23andMe results. This appears to be a family trend, go-figure a lot of my family also have type-2-diabetes mellitus (T2DM); low SHBG is a contributor to the development of T2DM. So, for those of us in urgent need of raising SHBG, what could help? Thyroid replacement therapy!
As mentioned, T3 can increase SHBG production at the liver. This is demonstrable in clinical studies; T3 increases SHBG. I can’t provide myself as a clinical use case I’m afraid – my thyroid is also naturally a bit on the higher side, so I don’t qualify for treatment. This reinforces the point that we should only prescribe T3 if it isn’t already optimal. Risking hyperthyroidism is downright stupid and dangerous. Many men with low SHBG tend to have low/normal levels of serum T3 and so could be supplemented to a more optimal (within range) level of T3 to increase SHBG, by a prescribing experienced medical professional. The benefits could outweigh the potential risks as it is necessary to have normalised SHBG, as highlighted in my previous article on SHBG.
Please tread cautiously with the use of thyroid hormones and have a full discussion with your prescribing medical clinician. While the thyroid gland (in those who have an otherwise functional gland) will bounce back to normal in most cases, there are significant risks to be considered should your T3 and T4 increase too much. Your individual response may be different; you may experience hyperthyroidism at lower levels of thyroid hormones than others, so you must bear this in mind and note any adverse symptoms and report them back to your doctor. It is down to your doctor to decide what is best for you.
Conclusions
Aside from both starting with the letter ‘T’, the thyroid and testes have more of a relationship than most realise. Hypogonadism can be largely caused by hypothyroidism, where treatment can reverse hypogonadism. Conversely, excessively high Testosterone could cause hyperthyroidism (this is more the case in supraphysiological levels). Thyroid hormones also drive the production of SHBG up, so it could serve as a potential route to increase SHBG in those with low SHBG. But this must be at the discretion and expert medical supervision of an experienced clinician who will monitor you closely. Isn’t it fascinating just how closely intertwined many processes in our bodies are?
References
- Nadri F, Khavanin A, Mazaheri Z, Soleimanian A. Effect of noise pollution on male fertility (Review). J Occup Heal Epidemiol. 2016;5(1):53-62. doi:10.18869/ACADPUB.JOHE.5.1.53
- Comninos AN, Jayasena CN, Dhillo WS. The relationship between gut and adipose hormones, and reproduction. Hum Reprod Update. 2014;20(2):153-174. doi:10.1093/HUMUPD/DMT033
- Skorupskaite K, George JT, Anderson RA. The kisspeptin-GnRH pathway in human reproductive health and disease. Hum Reprod Update. 2014;20(4):485-500. doi:10.1093/HUMUPD/DMU009
- Your thyroid gland | British Thyroid Foundation. https://www.btf-thyroid.org/what-is-thyroid-disorder. Accessed October 9, 2021.
- Context | Thyroid disease: assessment and management | Guidance | NICE.
- Underactive thyroid (hypothyroidism) – Causes – NHS. https://www.nhs.uk/conditions/underactive-thyroid-hypothyroidism/causes/. Accessed October 9, 2021.
- Overactive thyroid (hyperthyroidism) – Causes – NHS. https://www.nhs.uk/conditions/overactive-thyroid-hyperthyroidism/causes/. Accessed October 9, 2021.
- AW M. The interrelationships between thyroid dysfunction and hypogonadism in men and boys. Thyroid. 2004;14 Suppl 1(SUPPL.1). doi:10.1089/105072504323024552
- Crawford M, Kennedy L. Testosterone replacement therapy: Role of pituitary and thyroid in diagnosis and treatment. Transl Androl Urol. 2016;5(6):850-858. doi:10.21037/TAU.2016.09.01
- Mani Maran RR, Arunakaran J, Aruldhas MM. T3 Directly Stimulates Basal Testosterone and Oestradiol Cells in vitro and Modulates LH Induced Production by Rat Leydig. Endocr J. 2000;47(4):417-428.
- RR M. Thyroid hormones: their role in testicular steroidogenesis. Arch Androl. 2003;49(5):375-388. doi:10.1080/01485010390204968
- G B, P B, M S, et al. Characterization of sex hormone-binding globulin isoforms in hypothyroid women. Thyroid. 2002;12(2):101-105. doi:10.1089/105072502753522329
- A surprising diagnosis in a man with high testosterone levels | ICEECE2012 | 15th International & 14th European Congress of Endocrinology | Endocrine Abstracts. https://www.endocrine-abstracts.org/ea/0029/ea0029p1068. Accessed October 9, 2021.
- Becker U, Gluud C, Bennett P. The effect of oral testosterone on serum TBG levels in alcoholic cirrhotic men. Liver. 1988;8(4):219-224. doi:10.1111/J.1600-0676.1988.TB00996.X
- Eriksson AL, Lorentzon M, Mellström D, et al. SHBG Gene Promoter Polymorphisms in Men Are Associated with Serum Sex Hormone-Binding Globulin, Androgen and Androgen Metabolite Levels, and Hip Bone Mineral Density. J Clin Endocrinol Metab. 2006;91(12):5029-5037. doi:10.1210/JC.2006-0679
- Ohlsson C, Wallaschofski H, Lunetta KL, et al. Genetic Determinants of Serum Testosterone Concentrations in Men. PLoS Genet. 2011;7(10). doi:10.1371/JOURNAL.PGEN.1002313