The Endocrine System & Sleep

Humans, and many other animals, physiologically need enough sleep. Sleep is essential for us, as anyone with sleep deprivation can attest to. The detrimental long-term effects of sleep deprivation have been made into common knowledge by media and health organisations across the world.
But while you may know that not enough sleep is bad for you, you may not know what exactly it does to your endocrine system. I will be talking specifically about that in this blog.
Zzzz… The Circadian Rhythm & Your Sleep
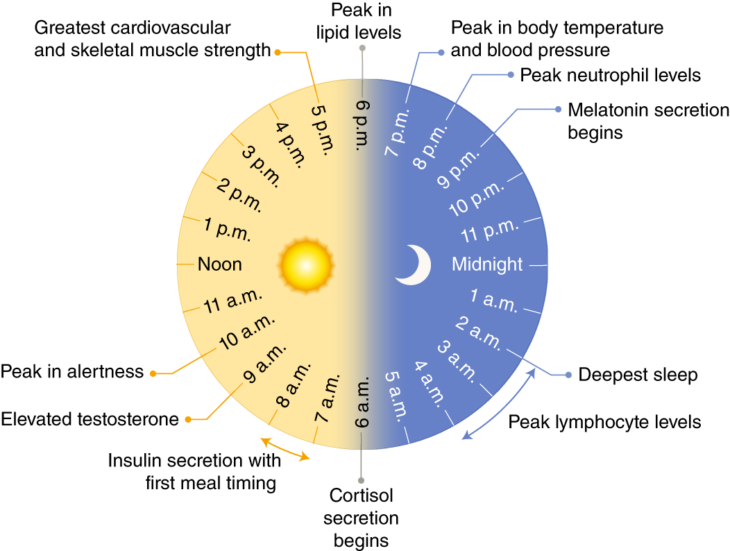
The circadian rhythm is a naturally recurring 24-hour cycle comprised of different biological processes, even in the absence of light fluctuations (i.e. day and night). Light also plays an important role in regulating our hormones. Within this 24 hour time period we have physiological changes throughout the day and night, as shown below (Masri and Sassone-Corsi, 2018) (click for full-size image):
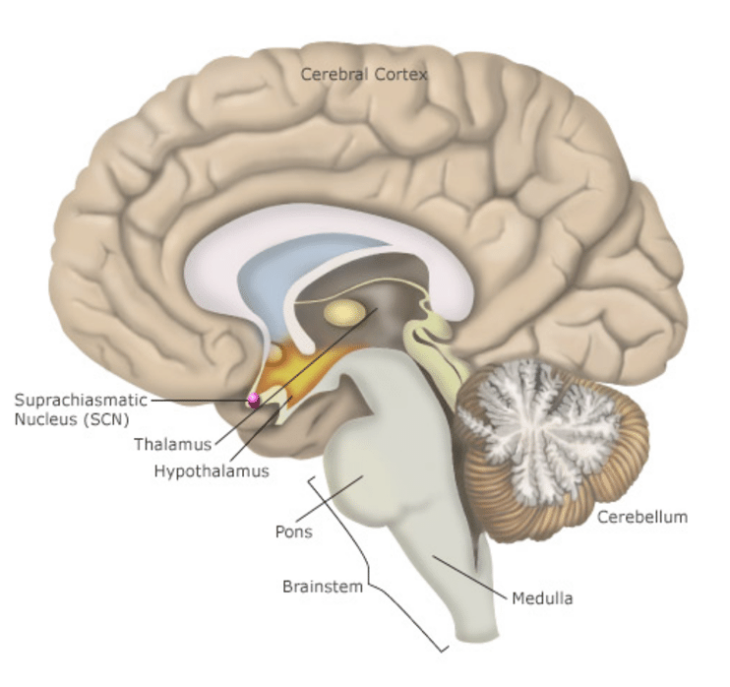
This is a completely autonomous (self-governed) mechanism that prepares to interact with external stimuli. It controls physiological processes from cortisol and sex steroid hormone release, to immune function and muscle strength. The major site of circadian control is in the suprachiasmatic nucleus (SCN), which is in the anterior (front) hypothalamus, sitting above the optic chiasm. This may be hard to visualise so I have included a drawing of the brain (sourced from Havard.edu) below (click for full-size image):
The cells of the SCN contain biological clocks. The SCN is referred to as the central clock; there exists a peripheral clock which is synchronized by the SCN. The entire mechanism by how these cells works is indeed very interesting, but complex and beyond the scope of this blog. Just know that they act as a ‘biological clock’, and the circadian clock can be adjusted depending on the amount and wavelength of light entering the retina, which travels along a path called the retinohypothalamic tract.
The SCN influences local peripheral clocks like those in the heart (controlling blood pressure), in the liver (controlling blood glucose and triglycerides), pineal gland (for releasing melatonin to make you feel sleepy), as well as the kidney (controlling clearance of waste, and timed release of glucocorticoids). It does this via the autonomic nervous system. It also helps regulate feeding behaviour and body temperature.
I’m sure you’ll agree that it’s pretty impressive you have this ‘master’ clock in your brain?! On the point of adjustment of this clock, you may have heard that blue light can keep you awake by preventing the production of melatonin; this is an example of light entering your retina that is altering your circadian cycle by way of the SCN.
So, for the insomniacs reading this, yes – blocking blue light can help resolve insomnia symptoms in some people (Shechter et al., 2018). If any electronic engineers are reading this, you may well know that LEDs (specifically white LEDs), also found in your phone, have peak wavelength emission in the blue light range – which not only causes issues with sleeping, but also damages the photoreceptor in your eyes. That’s one reason why using your phone, or laptop, just before bed may make it sometimes harder for you to fall asleep, and is generally not great for your health (Tosini et al., 2016).
Rapid eye movement (REM), and slow-wave sleep are also important factors in the circadian rhythm, which will have a knock on effect on hormonal and metabolic function (Tae Won Kim and Hong, 2015). Good quality sleep depends on numerous factors, but the circadian rhythm is one of them. That’s why alternate day/night shift working can make it difficult to achieve fully restful sleep; sleeping at a time other than what was normal will disrupt the circadian rhythm.
Circadian misalignment can cause several issues, including hormonal imbalance, i.e. low T and Cortisol, inflammation, and impaired glucose metabolism. This can increase the risk of obesity, metabolic syndrome, type II diabetes, gastrointestinal disease, cardiovascular disease, cancer risk, and other issues (James et al., 2017). This is an unfortunate price many pay for the dependence our 24/7 society has on shift work, prompting a dire need for countermeasures to be studied.
Sleep & Hormones
As mentioned, your hormones will fluctuate quite significantly throughout the 24-hour circadian rhythm. During sleep, certain hormones are secreted. But, for context, sleep is devised five stages. These include the following (Patel and Araujo, 2018):
Wake
If the eyes are open, alpha and beta waves are present, with beta being predominant (measured via an EEG – which measures the electrical activity in your brain as neurons are maintaining an electrical charge in your brain, changing it slightly with differing activity). As you become drowsy and close your eyes, the drowsy period, alpha waves will be predominant. You’ll begin to move towards light sleep.
Stage 1
This will be the light stage of sleep, your muscle tone and breathing will still be regular, alpha-waves are replaced with low-amplitude mixed-frequency activity in the brain. This lasts for 1-5 minutes and comprises ~ 5% of the total sleep cycle.
Stage 2
This will be the deeper stage of your sleep, your heart rate and body temperature drop, there’s more delta waves present (high amplitude). This is known as the slow-wave sleep stage and characterises deepening sleep. It lasts ~25 minutes and increases in length with each cycle, comprising 50% of the sleep cycle.
Stage 3
This is the deepest stage of sleep, with many lower frequency and higher amplitude delta waves. It’s difficult to awaken from this stage, and for those among us that sleep like logs, not even loud noises can awaken them during this phase. The older you get, the less time you spend during this stage. If you awake from this stage, you may have some mental fogginess, and tend to have moderately impaired mental performance for 30 minutes to an hour. This is the most important stage of your sleep for repair of your tissues; muscles and bones are grown in this stage, and the immune system is strengthened.
REM Sleep
Probably the most well-known and talked about stage of sleep. This stage is where dreaming occurs, eyes and breathing muscles will move rapidly, but your skeletal muscles are atonic (they will not move). This usually starts 90 minutes after falling asleep and typically lasts 10 minutes; the final REM stage can last up to an hour.
The 4 major sleep stages repeat until you’re awake. Those with sleep problems may struggle to reach deeper sleep stages, i.e. due to upper airways collapsing (sleep apnoea) and interfering with normal breathing, pushing them into lighter sleep to continue better breathing.
During your sleep, growth hormone (GH) levels are increased and peak during slow-wave sleep (Cauter et al., 1992). This hormone is secreted intermittently. Those with PTSD often have disturbed sleep and have lower serum levels of night-time and daytime (GH) as a result (Van Liempt et al., 2011). This may in part explain the decrease in GH as we age; we do not go into deeper sleep as often.
Melatonin is highest at night, versus day, and plays a very important role in regulating sleep. It reduces sleep latency, increases total sleep time, and improves sleep maintenance; this contributes to better quality sleep (Sharkey et al., 2001; Aeschbach et al., 2009). Melatonin production increases in the evening and peaks in the middle of the night, dropping to normal daytime low levels in the early morning. As mentioned, artificial light, especially blue light (or white LED light) can disrupt melatonin production.
Thyroid stimulating hormone (TSH) also reaches its maximum concentration in the middle of the night. Though a negative correlation between TSH levels and slow wave sleep (SWS) stage sleep is apparent; elevated TSH can cause worsening sleep quality. Free T3 does appear to increase thereon in the night, peaking at about 4am in a normal circadian rhythm (Russell et al., 2008).
Cortisol is well known to play a crucial role in the circadian rhythm, increasing rapidly in the middle of the biological night and then peaking in the morning, helping you awaken. It’s released in a pulsatile manner, in a 24-hour period, though increased cortisol decreases REM sleep, but increases SWS sleep (Tae Won Kim and Hong, 2015).
Testosterone and oestradiol, in natural healthy men, also has circadian variation. It peaks during sleep, due to an increase in pulsatile lutenising hormone (LH) secretion during sleep. This increase requires at least three hours of sleep, where the peak is established. It is known that low testosterone can affect overall sleep quality, worsening it, as can supraphysiological levels (Wittert, 2014). Disruptions in sleep can indeed lower the concentrations of testosterone and resulting oestradiol, hence why sleep apnoea is a major cause of hypogonadism. Likewise, this may explain why ageing trends towards decreases in testosterone concentration; poorer sleep quality will equate to reduced LH pulse peaks, and thus lower testosterone and thus oestradiol. Couple this with the fact that more older men tend to be overweight, a common risk factor for sleep apnoea (where age already increases the risk of sleep apnoea), and we thus see increased risk of hypogonadism (Bixler et al., 1998).
Sleep & Metabolism
We also see circadian rhythmic changes with your glucose and lipid metabolism. Glucose use is higher during physical activity and during waking hours versus sleep; expected due to increased energy demands. But there appears to be circadian regulation too; with variations that appear to be consistent in a 24-hour cycle. This is due to a combination of genetic, circadian clock, and hormonal regulation (Tae Won Kim and Hong, 2015).
Lipid absorption increases and decreases during high and low activity periods, respectively. The disruption of the circadian clock encourages the accumulation of triglycerides in adipose tissue and adipocyte hypertrophy, due to alteration in the activity of certain ‘fat’ related genes, proteins, and enzymes (Shostak et al., 2013) ; not adhering to your natural circadian clock encourages fat gain! This may in part explain the increased weight gain seen among shift workers. Additionally, your fat cells secrete adipokines, adiponectin, leptin, and plasminogen activator inhibitor 1 in a rhythmic manner with the circadian rhythm. This affects immune function, serum cholesterol levels, triglycerides, inflammation, and blood pressure. Dysregulation of the circadian rhythm, by way of lack of sleep or inconsistent sleep routines, and thus your fats ability to function as an effective endocrine organ, can risk elevated cholesterol, blood glucose, blood pressure, cardiovascular disease, worsened inflammatory responses, and type 2 diabetes mellitus (Gimble and Floyd, 2009). An increase in fat, to the point of obesity, can further reduce sleep quality via sleep apnoea, causing a vicious cycle.
The Effect of Sleep Deprivation on Hormones & Metabolism
As mentioned, sleep deprivation has many negative effects on your overall metabolic and hormonal health. Even in toddlers, sleep deprivation of less than 10.5 h/day can increase their obesity risk at 7 years of age! (Reilly et al., 2005). A universal trend seen across all ages is an increased risk of obesity and visceral fat accumulation with sleep deprivation (Tae Won Kim and Hong, 2015). As you’ve therefore guessed, it’s also a large risk factor for developed type 2 diabetes mellitus. Healthy men restricted to four hours per night of sleep for 6 nights, followed by 7 nights of 12 hours recovery sleep showed greatly reduced insulin sensitivity and thyrotropin. In addition to this, evening cortisol concentration and sympathetic nervous system activity was greater in the evening, with leptin levels being lower, while sleep deprived (Spiegel et al., 2005). This may lead to increased anxiety and appetite. Many studies, across a variety of different populations, also demonstrate that sleep restriction risks metabolic syndrome (Tae Won Kim and Hong, 2015). Even a sleep restriction of 6.5 hours in adolescents and adults lead to worsened health outcomes, with increase ghrelin (a hunger-related hormone), a large increase in hunger, appetite, and calorie consumption (Tae Won Kim and Hong, 2015). Furthermore, reduced sleep will thus reduce the number of sleep cycles and thus reduce sleep quality.
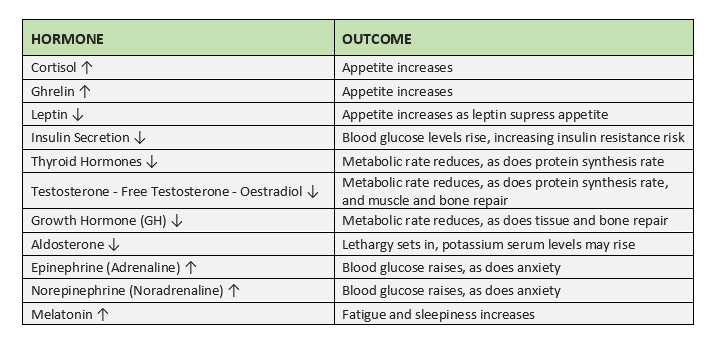
So, sleep deprivation is bad. To summarise, I’ve included the table below (Joo et al., 2012; Tae Won Kim and Hong, 2015):
Table 1 – Effects of sleep deprivation on hormones and the relative outcomes (click for full-size image)
The above demonstrates what happens in the 24 hours of sleep deprivation, these effects worsen with chronic sleep deprivation.
If you’re on Testosterone Replacement Therapy (TRT), a decrease in sex steroid hormones isn’t as much of a worry. But obviously, a decrease in all other health regulatory hormones and the adverse outcomes on your metabolism are a worry! Sleep deprivation can greatly damage your physical and mental health, and the positive outcomes of your TRT. Though shift work can negatively impact the circadian rhythm, adequate sleep will be essential to you no matter what medication you’re on, and adequate sleep combined with exercise and good diet will help negate some of the negative effects experienced with shift work.
How Can I Have Better Sleep?
Exercise can greatly improve sleep quality at all ages (Banno et al., 2018). Several techniques also help to encourage relaxation and induce sleep sooner, including the following (Insomnia: Relaxation techniques and sleeping habits – InformedHealth.org – NCBI Bookshelf):
- Progressive Muscle Relaxation – Where you flex groups of your muscle all over the body and then relax them again.
- Autogenic Training (AT) – Where you focus on the awareness of different parts of your body and consciously relax them.
- Imagery Visualisation – Visualising yourself in a peaceful, pleasant scene, or imagining yourself breathing quietly, will help with falling asleep sooner.
- Mindfulness Meditation – Where you focus on bringing your attention to the experiences that are occurring in the present moment, without thinking of them. Several apps exist to help guide your through this on the Apple app and Google play store.
Sleep hygiene can also have a profound positive effect on sleep quality and ability to fall asleep. This includes the following:
- Not drinking alcohol, coffee, or caffeine containing teas (in addition to other stimulates) four to six hours before bed.
- Avoiding smoking before bedtime or during the night.
- Avoiding heavy meals and spicy/hot foods before going to bed.
- Increase the amount of daytime exercise but try avoiding exercise right before bed.
- Ensure your room is quiet, dark, not too hot, or too cold.
- Leave your room so that it is primarily associated with sleep (or sex), i.e. don’t turn your room into a cinema or office, if possible.
- Try to have a consistent sleep routine.
Cognitive behavioural therapy may also be effective if you suffer from insomnia. However, a sleep study may be warranted if you suspect sleep apnoea, which is characterised by loud snoring, being tired throughout the day and choking in your sleep. If you experience constant fatigue and you sleep with a partner, ask them if you’ve been snoring loudly as this may also warrant a sleep study. At The Men’s Health Clinic we offer sleep studies, CPAP therapy and full sleep support services through our professional partnership with Phillips. Check out our Sleep Health page for more information.
References
- Aeschbach,D. et al. (2009) Use of transdermal melatonin delivery to improve sleep maintenance during daytime. Pharmacol. Ther., 86, 378–382.
- Banno,M. et al. (2018) Exercise can improve sleep quality: A systematic review and meta-analysis. PeerJ, 2018.
- Bixler,E.O. et al. (1998) Effects of age on sleep apnea in men. I. Prevalence and severity. J. Respir. Crit. Care Med., 157, 144–148.
- Cauter,E. Van et al. (1992) A quantitative estimation of growth hormone secretion in normal man: Reproducibility and relation to sleep and time of day. Clin. Endocrinol. Metab., 74, 1441–1450.
- Gimble,J.M. and Floyd,Z.E. (2009) Fat circadian biology. Appl. Physiol., 107, 1629–1637.
- Insomnia: Relaxation techniques and sleeping habits – InformedHealth.org – NCBI Bookshelf.
- James,S.M. et al. (2017) Shift Work: Disrupted Circadian Rhythms and Sleep—Implications for Health and Well-being. Sleep Med. Reports, 3, 104–112.
- Joo,E.Y. et al. (2012) Adverse effects of 24 hours of sleep deprivation on cognition and stress hormones. Clin. Neurol., 8, 146–150.
- Van Liempt,S. et al. (2011) Decreased nocturnal growth hormone secretion and sleep fragmentation in combat-related posttraumatic stress disorder; potential predictors of impaired memory consolidation. Psychoneuroendocrinology, 36, 1361–1369.
- Masri,S. and Sassone-Corsi,P. (2018) The emerging link between cancer, metabolism, and circadian rhythms. Med., 24, 1795–1803.
- Patel,A.K. and Araujo,J.F. (2018) Physiology, Sleep Stages StatPearls Publishing.
- Reilly,J.J. et al. (2005) Early life risk factors for obesity in childhood: Cohort study. Med. J., 330, 1357–1359.
- Russell,W. et al. (2008) Free triiodothyronine has a distinct circadian rhythm that is delayed but parallels thyrotropin levels. Clin. Endocrinol. Metab., 93, 2300–2306.
- Sharkey,K.M. et al. (2001) Effects of melatonin administration on daytime sleep after simulated night shift work. Sleep Res., 10, 181–192.
- Shechter,A. et al. (2018) Blocking nocturnal blue light for insomnia: A randomized controlled trial. Psychiatr. Res., 96, 196–202.
- Shostak,A. et al. (2013) Circadian regulation of lipid mobilization in white adipose tissues. Diabetes, 62, 2195–2203.
- Spiegel,K. et al. (2005) Sleep loss: A novel risk factor for insulin resistance and Type 2 diabetes. Appl. Physiol., 99, 2008–2019.
- Tae Won Kim,J.-H.J. and Hong,S.-C. (2015) The Impact of Sleep and Circadian Disturbance on Hormones and Metabolism. J. Endocrinol.
- Tosini,G. et al. (2016) Effects of blue light on the circadian system and eye physiology. Vis., 22, 61–72.
- Wittert,G. (2014) The relationship between sleep disorders and testosterone in men. Asian J. Androl., 16, 262–265.