TRT, SHBG & Health – Facts, Questions and Evolution
If you’re on TRT, you’ve more than likely heard of sex hormone binding globulin (SHBG). But have you wondered what it is, what it does, and how it affects our health? In this blog, I will detail exactly that, outlining what we know, what we can speculate, and from that – how we can potentially manage it.
What is SHBG, Actually?
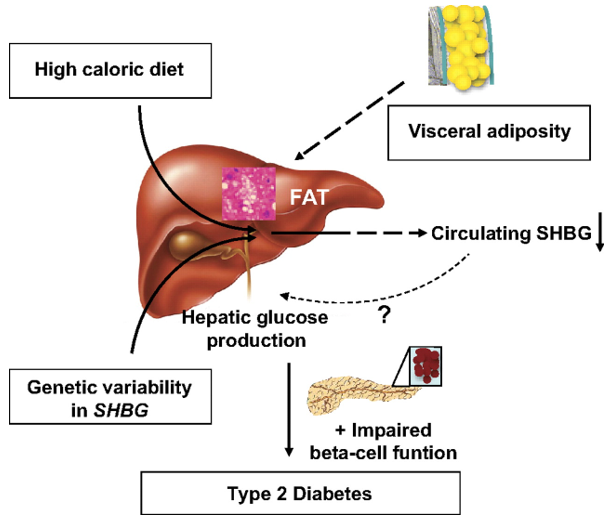
SHBG is a glycoprotein that’s made in your liver which binds to androgens and oestrogens, namely your sex-steroid hormones. Of most importance, it binds to dihydrotestosterone (DHT), testosterone, and oestradiol. This is true for both women and men. Interestingly, DHT has the highest binding affinity to SHBG, likely due to the additional hydrogen bond it has, followed by Testosterone and then Oestradiol 1. It can be affected by several things, including a high calorie diet, genetic variability, and visceral adiposity. It also has downstream effects on impairing beta cell function is SHBG is too low (we’ll discuss this further). This is well shown in Figure 1, below (click for full-size image):
Figure 1 – Hypothetical picture regarding cause and metabolic consequences of circulating SHBG in humans 2
When circulating in the bloodstream, Testosterone, DHT, and Oestradiol will mostly be loosely bound to serum albumin and some will be bound tightly to SHBG, with only a small amount of the hormones being unbound, or ‘free’. Serum albumin is the most abundant protein in our blood plasma, and has a range of functions that aren’t just limited to steroid hormone transport, owed to its highly flexible 3-domain structure 3. In-fact, approximately 53-55% of Testosterone is bound to serum albumin, and 43-45% bound to SHBG, though this of course varies person to person 3.
You may have noticed I mentioned that the sex hormones will loosely bind to serum albumin, versus a tight binding with SHBG. This correlates to the rate of release of sex steroid hormones, where SHBG will release testosterone less rapidly than albumin; albumin simply acts as a reservoir for sex-steroid hormones, and it can rapidly regulate local serum testosterone concentrations in the blood 3. As total Testosterone increases, we tend to see an increase in SHBG. Conversely, with low total testosterone, we tend to see a decrease in SHBG. This is likely to maintain a more stable level of free Testosterone.
On the topic of albumin, it’s suspected that an increase in fatty acid concentrations will increase the binding strength of serum albumin with Testosterone and thus alter bioavailability; perhaps an important consideration for those with high triglycerides or those dieting, particularly with a ketogenic diet 4. This may see to a larger decrease in total testosterone if your SHBG is also high. However, this remains a controversial topic and irrespective of this, those on TRT will see suppression of regulatory enzymes that synthesise fatty acids and otherwise protect against hepatic steatosis (fatty liver) and generally decrease fat mass 5,6.
So, you’ve probably already guessed that SHBG and albumin are both very important in the regulation of bioavailable testosterone concentrations. We will be focusing on SHBG in further detail in this blog and now some questions might start to also appear in your mind, ranging from whether low or high SHBG is better. So, how does our SHBG concentrations actually affect our health?
Causes of High & Low SHBG
High SHBG
Several causes exist, and among them Anorexia is one. Anorexia observes a negative energy balance, i.e. the same as being in a hypocaloric diet (eat less than you should – but to an extreme), which also causes an increase in SHBG 7 and this is likely due to the downregulation of androgen production in a bid to reduce energy costly intensive anabolic processes that they stimulate, such as muscle and bone growth. Perhaps another explanation can be due to increased liver production of SHBG due to a reduction in net energy balance, detected by the liver.
Hyperthyroidism is another cause, where thyroid hormones are known to increase SHBG by directly altering the production of SHBG in the hepatocytes (liver cells), likely due to thyroid hormones increasing gene expression of HNF-4α within the liver, where HNF-4α increases SHBG production. This also provides some evidence for why anorexia may contribute to elevate SHBG. For those curious what HNF-4α does, well it plays a very key role in the transcriptional activity of the SHBG promoter region 8 – as its activity increases, so does SHBG production.
We also see high SHBG in those with liver disease, due to improper hepatocyte function, those with growth hormone deficiency, the elderly/ageing, androgen deficiency (potentially due to reduced free oestradiol levels leading to altered liver function 9.), and genetic mutations in the SHBG gene 10.
Low SHBG
Among causes of low SHBG exist obesity, particularly with increased visceral fat which is likely due to increased leptin production which is a hormone produced by fat cells 11. The more fat you carry, the more leptin you produce.
Type 2 diabetes mellitus (T2DM) is another cause, likely due to insulin resistance, which may arguably be controlled by visceral fat and thus leptin, again – as insulin increases, so does leptin, which aims to decrease insulin produced by the pancreas and also reduce appetite via leptin receptors in the brain 12. Hypothyroidism can also cause low SHBG, for reason as you’ve probably guessed relates to a lack of HNF-4α stimulation; another reason why hypercaloric diets can also lower SHBG. Excess growth hormone also causes low SHBG, as does Cushing’s disease, non-alcoholic fatty liver disease, and excessively high Testosterone and Oestradiol.
SHBG & Your Health
First, we need to be clear that SHBG is not only important for transporting sex steroids. SHBG can impact health in various ways, but mechanisms also exist in place to prevent negative outcomes associated with altered SHBG. For example, SHBG will reduce cellular uptake of testosterone and thus impact health in different ways. For example, if reducing SHBG, excess free Testosterone may enter cells and thus oversaturate androgen receptors, particularly in the prostate which can contribute to benign prostate hypertrophy 13. Though, much of this testosterone will be conjugated (bound) to glucuronic acid (sugar made from glucose, also found in gum) in the prostate and then effluxed (flows out), with a decrease in androgen receptor density following this due to the androgen receptor oversaturation, leading to a less ‘androgen sensitive’ prostate. This is a protective effect against benign prostate hypertrophy, though unrelated to potential cancer growth which is indeed related to Oestradiol as mentioned in my previous Oestradiol blog.
There also exists a specific SHBG receptor which binds to SHBG and has effects downstream of it, much of which are yet to be investigated. But, to bind to the SHBG receptor, the SHBG must be unbound to a sex-steroid 14. This is a consideration not even discussed in depth here as we just don’t know enough studies to say what happens. So, lets dive into what high and low SHBG can do to your health.
High SHBG
Certain SHBG mutations that elevate SHBG are known to be negatively correlated with type 2 diabetes (T2DM), where high circulating SHBG can prevent the development of T2DM without altering insulin secretion, but instead via regulating fasting blood sugar. Interestingly, we find that SHBG levels do correlate positively with insulin sensitivity 2… but is this correlation and causation? Insulin is known to impair liver insulin production and insulin resistance can lead to large increases in insulin secretion, thus a lower SHBG may be present 15.
But remember I mentioned a mutation in the SHBG gene improves T2DM risk? This data specifically comes from 15 studies with over 27,657 T2DM cases and 58,481 control populations; the single nucleotide polymorphism (SNP – a single base change in an allele of a gene that can have enormous changes in the gene expression) rs1799941,was shown to be associated with a 95% (91-99%) and 93% (89-98%) protective effect against T2DM development in men and women, respectively. This relationship exists even when controlling for body fat and yet no associations were found between this SNP/mutation and insulin resistance or secretion, thus suggesting the SHBG plays a very essential role in preventing T2DM and protecting us from certain bad metabolic profiles that can increase the risk of other diseases like cardiovascular heart diseases (CVD) 16–18.
So, in short – high SHBG can be a good thing and protect us from T2DM and cardiovascular diseases. This is further backed up by independent studies, including studies using young men (2716 men aged 31 yrs), where higher SHBG concentrations are shown to improve cardiovascular risk profiles independent of total testosterone 19. Naturally, with reduced CVD and T2DM risk, we’d expect to see a decline in dementia risk, though Muller et al., demonstrated the converse in elderly populations , where increased SHBG appears to be associated with dementia, independent of CVD risk factors and bioactive hormone levels 20. However, it’s still to be elucidated if SHBG is casually related to dementia, as this is an elderly population where the risk of dementia nonetheless will be higher. There is suggested involvement of SHBG with the brains neurophysiology and perhaps neuropathology 21. Don’t panic if you’ve high SHBG; it needs further elucidation what its role in the brain actually is. We do however know that it will improve your metabolic profile.
However, it’s been observed that with a subjectively high serum SHBG, we note an increased vertebral fracture risk, independent of bone mineral density, among elder men 22. This is likely a result of decreased bioavailable Testosterone and Oestradiol, and this may explain why some patients observe androgen deficient symptoms when they have normal total testosterone and oestradiol but very high SHBG. In addition to this, there may be a relationship between gastric cancer and elevated SHBG, where patients with gastric cancer have elevated SHBG, but whether SHBG being elevated increases risk of gastric cancer is unclear 23. It may be that gastric cancer causes an increase in SHBG, though in the study that identified this causal relationship among women, it was postulated that it’s due to lowered free Oestradiol, which has a protective effect against gastric cancer 23.
Nonetheless, we first need to rule out other causes of high SHBG before concluding that it’ll have a protective effect. These causes include androgen deficiency, anorexia, growth hormone deficiency, and hyperthyroidism, as these are problematic disorders. Furthermore, elevated SHBG that’s too high in men with low-normal total Testosterone can risk very low free sex steroid hormones and potentially cause androgen deficiency symptoms.
Low SHBG
Lower levels of SHBG in younger men have been associated with an increase in non-alcoholic fatty liver disease in middle age, in addition to increased visceral adiposity (bad organ covering fat) 24. Obesity is also well associated with lower SHBG and this doesn’t appear to be a matter of correlation and causation, either 25. Also, as realized from high SHBG having a protective effect against poor metabolic profiles, low SHBG is well associated with cardiovascular diseases, T2DM, and comorbidities. Additionally, high free testosterone and DHT have been identified to increase the risk of developing Barrett’s oesophagus (acid reflux) by 436%, in men; but no direct mechanism is understood 26. Further studies are needed before we conclude DHT and testosterone to be a cause of acid reflux, which is important to elucidate as it can develop into oesophageal cancer.
Ironically, with supraphysiological androgen levels we tend to see an increase in fasted blood sugar and insulin resistance, and a decrease in SHBG. Perhaps this is a cause of lowered SHBG with excessive Testosterone use, or perhaps the low SHBG leads to worsened insulin sensitivity; a topic worth elucidating in future studies. Regardless, this is very important as poor insulin sensitivity is associated with innumerable comorbidities (other diseases).
So – high SHBG is all protective, whereas low SHBG appears to not be protective – right? Well, the consensus is overwhelmingly clear; a higher SHBG is protective against many diseases. But, we still need to pay careful attention to total and free circulating sex-steroid hormones alongside serum albumin, fasted blood sugar, HbA1C, and symptoms before we can determine if SHBG needs lowering, or raising, respectively. I’ve only shown a snippet of a few large-scale studies and metanalysis; there are plenty more studies that demonstrate this protective effect and none to the contrary, with only a few suggesting poor outcomes with high SHBG, regarding certain diseases such as dementia in the elderly.
SHBG & Sex Steroid Hormone Interacts – Natural Trends?
Interestingly, we do see that a significant rhythm existing in young eugondal (healthy natural) men; the acrophase (peak) of SHBG generally occurs in the mid-afternoon at ~15:00 hrs, whereas total and free testosterone demonstrate peaks in the early morning at around 7:00 – 7:30 hrs. This would correlate with the peak and troughs we see with testosterone, where it trends towards a rapid decline at roughly when SHBG increases, and then a small increase in TT again before a large decline, as shown by Figure 2 below (click for full-size image):
Figure 2 – Diurnal rhythm of testosterone in elderly and young men 27
We would suspect that, during this time, we may see a decline in testosterone and oestradiol stimulated anabolic activity, though their effects will be primarily seen regardless due to their prior large increase earlier in the day (the effect is predominantly gene mediated; whether we are anabolic or not is largely controlled by how we eat through the day and our metabolic profile).
SHBG & Age – Evolution or Coincidence?
Interestingly, elderly men with higher SHBG are less likely to suffer from pathologies associated with metabolic syndrome and may well likely live longer 28.
What else do we notice in old people? An increase in SHBG! This is concurrent with a decline in total testosterone 29. This is likely due to testicular dysfunction 30; aging is in general associated with degeneration of various organ systems, with the rate at which this occurs depending on genetics, existing diseases, and the accumulative effects of socioeconomic, lifestyle, and environmental factors. Why may this occur? Well, cells are aging and have either exhausted the number of cell cycles that they have left to undergo mitosis (Hayflick constant, approximately 50 cell cycles), and telomeres shorten. Telomeres are regions containing many nucleotide sequences at the end of a chromosome, which basically act a reservoir to produce extra base ‘coding’ units for when a cell replicates via mitosis. This shortening of the telomere increases genomic instability, meaning cells are more likely to become cancerous… or just die. This may explain why the testicles begin to lose function. But why do we see an increase in SHBG if it’s meant to decrease when we have low total testosterone?
Well, it may be in an attempt to compensate for serum albumin, which tends to decline with age, potentially due to worsened liver function 31, but the answer isn’t clear. Humans haven’t historically been living for as long as they do now with the aid of good hygiene, better food access, improved lifestyles, and modern medicine; thus, this likely isn’t a question that could be answered by means of evolution. So, to answer a question on why old people have elevated SHBG is one that needs more research. Nonetheless, this rise in SHBG is not to be feared with old age as it may well prove helpful to the extension of your lifespan. But, we should also consider quality of life, and so if any androgen deficiency symptoms are present, then provided the patient is in good health, we may need to provide some form of androgen treatment; but this MUST be discussed with a doctor further, as always.
How Can We Control SHBG?
By now you may well be convinced that you want high SHBG, but if you aren’t a very old man, then I suspect you want optimal SHBG levels. This will need to be reviewed with your doctor based upon blood tests and symptoms. We can control SHBG by not using traditional TRT, which often sees a sudden drop in SHBG due to an acute large raise in Testosterone and subsequent sudden drop, leading to very high free sex-steroid concentrations. We can use micro-dosing to increase SHBG and we have observed this working in action in clinical practice. We can also lose bodyfat and improve our diets so that they contain less sugar and control our blood sugar better, as insulin will also lower SHBG.
For those not on TRT, if you have symptoms of low Testosterone, but have high SHBG, with no clinical indications for having hypogonadism, it may well be worth addressing your SHBG. Ascertain that it’s not high due to genetics, and that it’s not caused by a hypocaloric diet or any of the conditions mentioned in this blog for high SHBG. For those with low SHBG who are afraid their days are now numbered; don’t worry, again we need to rule out external causes, include hypercaloric diet and overweightness (both of which can be controlled); you can manage your low SHBG by using microdosing, and if your testosterone and HCG dose is too high; lower it – but only after speaking with your supervising Doctor and under their consultation.
References
- Grishkovskaya I, Avvakumov G V., Sklenar G, Dales D, Hammond GL, Muller YA. Crystal structure of human sex hormone-binding globulin: Steroid transport by a laminin G-like domain. EMBO J. 2000;19(4):504-512. doi:10.1093/emboj/19.4.504
- Peter A, Kantartzis K, Machann J, et al. Relationships of circulating sex hormone-binding globulin with metabolic traits in humans. Diabetes. 2010;59(12):3167-3173. doi:10.2337/db10-0179
- Czub MP, Venkataramany BS, Majorek KA, et al. Testosterone meets albumin-the molecular mechanism of sex hormone transport by serum albumins. Chem Sci. 2019;10(6):1607-1618. doi:10.1039/c8sc04397c
- Manni A, Pardridge WM, Cefalu W, et al. Bioavailability of albumin-bound testosterone. J Clin Endocrinol Metab. 1985;61(4):705-710. doi:10.1210/jcem-61-4-705
- Kelly DM, Nettleship JE, Akhtar S, et al. Testosterone suppresses the expression of regulatory enzymes of fatty acid synthesis and protects against hepatic steatosis in cholesterol-fed androgen deficient mice. Life Sci. 2014;109(2):95-103. doi:10.1016/j.lfs.2014.06.007
- Koutsari C, Ali AH, Nair KS, et al. Fatty acid metabolism in the elderly: Effects of dehydroepiandrosterone and testosterone replacement in hormonally deficient men and women. J Clin Endocrinol Metab. 2009;94(9):3414-3423. doi:10.1210/jc.2009-0165
- Cangemi R, Friedmann AJ, Holloszy JO, Fontana L. Long-term effects of calorie restriction on serum sex-hormone concentrations in men. Aging Cell. 2010;9(2):236-242. doi:10.1111/j.1474-9726.2010.00553.x
- David M Selva and GLH. Thyroid hormones act indirectly to increase sex hormone-binding globulin production by liver via hepatocyte nuclear factor-4α in: Journal of Molecular Endocrinology Volume 43 Issue 1 (2009). Journal of Molecular Endocrinology. https://jme.bioscientifica.com/view/journals/jme/43/1/19.xml. Published 2009. Accessed February 5, 2020.
- Lu H. Crosstalk of HNF4α with extracellular and intracellular signaling pathways in the regulation of hepatic metabolism of drugs and lipids. Acta Pharm Sin B. 2016;6(5):393-408. doi:10.1016/j.apsb.2016.07.003
- Sex Hormone Binding Globulin | South Tees Hospitals NHS Foundation Trust. https://www.southtees.nhs.uk/services/pathology/tests/shbg/. Accessed February 2, 2020.
- Liu CC, Huang SP, Cheng KH, et al. Lower SHBG level is associated with higher leptin and lower adiponectin levels as well as metabolic syndrome, independent of testosterone. Sci Rep. 2017;7(1). doi:10.1038/s41598-017-03078-0
- Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. Narrative Review: The Role of Leptin in Human Physiology: Emerging Clinical Applications. Ann Intern Med. 2010;152(2):93. doi:10.1059/0003-4819-152-2-201001190-00008
- Li H, Pham T, Mcwhinney BC, et al. Sex Hormone Binding Globulin Modifies Testosterone Action and Metabolism in Prostate Cancer Cells. Int J Endocrinol. 2016;2016. doi:10.1155/2016/6437585
- Hryb DJ, Khan MS, Romas NA, Rosner W. The control of the interaction of sex hormone-binding globulin with its receptor by steroid hormones. J Biol Chem. 1990;265(11):6048-6054. http://www.ncbi.nlm.nih.gov/pubmed/2156840. Accessed February 2, 2020.
- Le TN, Nestler JE, Strauss JF, Wickham EP. Sex hormone-binding globulin and type 2 diabetes mellitus. Trends Endocrinol Metab. 2012;23(1):32-40. doi:10.1016/j.tem.2011.09.005
- Perry JRB, Weedon MN, Langenberg C, et al. Genetic evidence that raised sex hormone binding globulin (SHBG) levels reduce the risk of type 2 diabetes. Hum Mol Genet. 2009;19(3):535-544. doi:10.1093/hmg/ddp522
- Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591-604. doi:10.1038/s41574-018-0048-7
- Leon BM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6(13):1246. doi:10.4239/wjd.v6.i13.1246
- Canoy D, Barber TM, Pouta A, et al. Serum sex hormone-binding globulin and testosterone in relation to cardiovascular disease risk factors in young men: A population-based study. Eur J Endocrinol. 2014;170(6):863-872. doi:10.1530/EJE-13-1046
- Muller M, Schupf N, Manly JJ, Mayeux R, Luchsinger JA. Sex hormone binding globulin and incident Alzheimer’s disease in elderly men and women. Neurobiol Aging. 2010;31(10):1758-1765. doi:10.1016/j.neurobiolaging.2008.10.001
- Caldwell JD, Suleman F, Chou SHH, Shapiro RA, Herbert Z, Jirikowski GF. Emerging roles of steroid-binding globulins. Horm Metab Res. 2006;38(4):206-218. doi:10.1055/s-2006-925328
- Vandenput L, Mellström D, Kindmark A, et al. High Serum SHBG Predicts Incident Vertebral Fractures in Elderly Men. J Bone Miner Res. 2016;31(3):683-689. doi:10.1002/jbmr.2718
- Cheng CW, Chang CC, Patria YN, et al. Sex hormone-binding globulin (SHBG) is a potential early diagnostic biomarker for gastric cancer. Cancer Med. 2018;7(1):64-74. doi:10.1002/cam4.1254
- Sarkar M, VanWagner LB, Terry JG, et al. Sex Hormone-Binding Globulin Levels in Young Men Are Associated With Nonalcoholic Fatty Liver Disease in Midlife. Am J Gastroenterol. 2019;114(5):758-763. doi:10.14309/ajg.0000000000000138
- Cooper LA, Page ST, Amory JK, Anawalt BD, Matsumoto AM. The association of obesity with sex hormone-binding globulin is stronger than the association with ageing – Implications for the interpretation of total testosterone measurements. Clin Endocrinol (Oxf). 2015;83(6):828-833. doi:10.1111/cen.12768
- Cook MB, Wood SN, Cash BD, et al. Association Between Circulating Levels of Sex Steroid Hormones and Barrett’s Esophagus in Men: A Case-Control Analysis. Clin Gastroenterol Hepatol. 2015;13(4):673-682. doi:10.1016/j.cgh.2014.08.027
- Bremner WJ, Vitiello M V., Prinz PN. Loss of circadian rhythmicity in blood testosterone levels with aging in normal men. J Clin Endocrinol Metab. 1983;56(6):1278-1281. doi:10.1210/jcem-56-6-1278
- Muller M, Grobbee DE, Den Tonkelaar I, Lamberts SWJ, Van Der Schouw YT. Endogenous sex hormones and metabolic syndrome in aging men. J Clin Endocrinol Metab. 2005;90(5):2618-2623. doi:10.1210/jc.2004-1158
- Liu PY, Beilin J, Meier C, et al. Age-related changes in serum testosterone and sex hormone binding globulin in Australian men: Longitudinal analyses of two geographically separate regional cohorts. J Clin Endocrinol Metab. 2007;92(9):3599-3603. doi:10.1210/jc.2007-0862
- Araujo AB, Wittert GA. Endocrinology of the aging male. Best Pract Res Clin Endocrinol Metab. 2011;25(2):303-319. doi:10.1016/j.beem.2010.11.004
- Gomi I, Fukushima H, Shiraki M, et al. Relationship between serum albumin level and aging in community-dwelling self-supported elderly population. J Nutr Sci Vitaminol (Tokyo). 2007;53(1):37-42. doi:10.3177/jnsv.53.37