TRT – Best Practice

Introduction
The Men’s Health Clinic is a CQC Registered private medical clinic that specialises in the diagnosis and management of men with Testosterone Deficiency. Lydia and I opened the clinic in January 2016. From very humble beginnings we now have our very own bespoke TRT clinic which brings in men from all over the world. We are very proud of what we have achieved, it has taken hard work, dedication, perseverance and many a sleepless night. We have always been fully transparent about our clinical practice, not only to build trust, but to hopefully to affect a positive change to how Testosterone Deficiency is approached in the UK. We aim to deliver the gold standard in every aspect of the care and service we provide. We offer a personalised service, focusing on the best interests of our patients. To affect a positive change to how low testosterone is perceived and managed in the UK, we need to raise awareness of its importance in overall health, we need to break down barriers that prevent progress, we need to stand tall for all to see.
NHS Guidelines vs BSSM Guidelines
We have always been fully transparent and open about how we practice and the rationale for adopting such practices. We adhere to the British Society for Sexual Medicine (BSSM) Guidelines on Adult Testosterone Deficiency, which are national guidelines to help clinicians manage and diagnose men with Testosterone Deficiency. The fact that we utilise these guidelines in our clinical practice is clearly documented on our clinic website. It is also repeatedly mentioned in blogs, YouTube Vlogs, and on other social media platforms.
The BSSM definition for Testosterone Deficiency is highlighted on the Testosterone Deficiency & Diagnosis page of our website. The following is a direct transcript from the guidelines:-
“A well-established and significant medical condition. It is defined as a clinical and biochemical syndrome associated with advancing age and comorbidities and is characterized by a deficiency in serum androgen levels (with or without decreased genomic sensitivity to androgens) and relevant signs and symptoms. Testosterone Deficiency can adversely affect multiple organ systems and result in significant decreases in quality of life, including changes in sexual function.”
This is in line with the Society for Endocrinology Position Statement on Male Hypogonadism and Ageing, written by Consultant Endocrinologist, Dr Richard Quinton:-
“Hypogonadism is defined as a clinical syndrome complex that comprises symptoms and signs as well as biochemical evidence of testosterone deficiency.”
There are NHS Endocrinologists who do not believe that ‘Testosterone Deficiency’ is a medical diagnosis. This goes against the position statement made by the Society for Endocrinology.
If it is necessary to identify an underlying organic pathology for low testosterone, then we should apply this same standard to other endocrine diagnoses such as Hypothyroidism and Type 2 Diabetes Mellitus, where there often isn’t an underlying organic pathology. According to the World Health Organisation, Depression is a disease state. The most commonly prescribed medication to treat depressive symptoms is a Selective Serotonin Reuptake Inhibitor (SSRI), a medication that increases expression of Serotonin within the brain. Low serotonin is not an organic pathology, it isn’t even a confirmed cause of depression. Quantitative markers are not measured pre-treatment, nor monitored whilst on treatment. Medications are prescribed in an attempt to reverse the negative symptoms of the disease state and prevent the long-term complications of the condition. A patient should not be denied treatment for a defined medical condition simply because a clinician cannot find an organic cause.
The National Institute for Clinical Effectiveness (NICE) has not produced guidance for Testosterone Deficiency or Male Hypogonadism. The BSSM guidance therefore provides clinicians with a national consensus on diagnosing and managing Testosterone Deficiency. These guidelines are in line with European Society for Sexual Medicine (ESSM) and International Society for Sexual Medicine (ISSM) guidelines. Whilst clinicians may have the right to differing opinions on what might be considered best practice, stating “in my opinion, ‘testosterone deficiency’ is not a diagnosis in itself” when there is evidence to the contrary, is rather presumptive and arrogant without sufficient justification. An alarming number of NHS Endocrinologists do not accept the validity of the BSSM guidelines, however, NHS hospital trusts such as James Paget University Hospitals, Norfolk and Norwich University Hospitals and The Queen Elizabeth Hospital King’s Lynn trust have formulated their own trust guidelines, where they have adopted the BSSM diagnostic criteria and reference ranges.
The BSSM’s diagnostic criteria laid out in their own current guidelines is clearly referenced on the Testosterone Deficiency & Diagnosis page of our website, as this is the diagnostic criteria that we adhere to. I have included the relevant excerpt below:-
“Serum T should be measured from 7 to 11 AM on at least 2 occasions with a reliable method preferably 4 weeks apart and, if possible, not during an acute illness.”
Regarding the thresholds for treatment intervention in symptomatic men, BSSM and ISSM guidelines recommend the following:
TT level lower than 8 nmol/L or FT level lower than 180pmol/L (<0.180 nmol/L; based on 2 separate levels from 8 to 11 AM) usually requires T therapy.
Levels from 8 to 12 nmol/L might require a trial of T therapy for a minimum of 6 months based on symptoms.
A FT level lower than 225 pmol/L (0.225 nmol/L) provides supportive evidence for T therapy in the presence of appropriate symptoms.”
Pathology Reference Ranges
The Men’s Health Clinic is an internationally recognised medical clinic, we have patients travel to our clinic from all over the world to be under our care and supervision. It is therefore necessary to have consistency in reporting and actioning blood markers.
As per the BSSM guidance and the Society of Endocrinology position statement on Testosterone Deficiency, the diagnosis of Testosterone Deficiency should be made based on persistent negative symptoms, along with confirmatory diagnostic bloodwork. However, there is still a clear emphasis on diagnostic blood test results, with over 80% of clinical diagnoses being made from laboratory testing(1)(2). A normal reference range “is an interval that, when applied to the population serviced by the laboratory correctly, includes most of the subjects with characteristics similar to the reference group and excludes the others.”(3). There is typically a 95% confidence interval applied to reference ranges, meaning that 5% of normal people will fall outside of the reference range.
There is also a lack of standardisation of the analytical methods used to determine reference ranges. The validity of these reference ranges is affected by factors such as the strength of the study, attaining adequate sample sizes to make the ranges statistically significant, inclusion and exclusion criteria and preanalytical sources of variation. You would also need to factor in that testosterone levels decrease with age(4)(5), and that average testosterone levels are dropping(6).
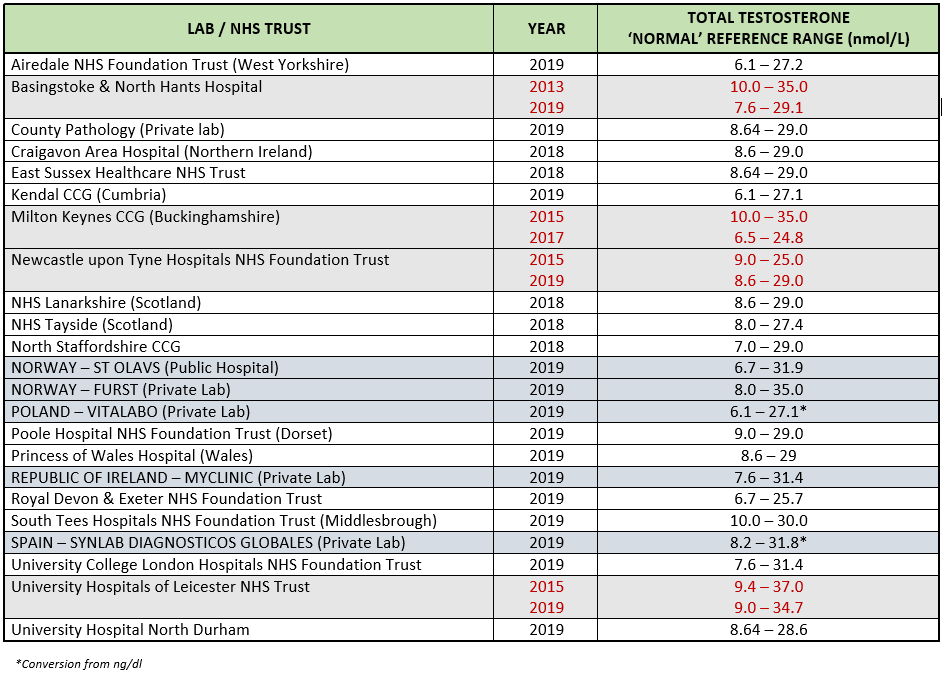
Regional variation in the purported “normal” testosterone reference range is an issue all over the UK. This further highlights the necessity for standardisation and a national consensus in ascribing to diagnostic criteria to avoid any confusion.
As you can see in the table below, there is both regional and national variation in what is considered normal. The table also highlights the disparity over time. The earlier claim that average testosterone levels are declining, is further supported by the lowering of up-to-date reference ranges. A drop in average testosterone levels with time most surely reflects a sick society, since we know that there are negative symptoms associated with a deficiency. Ageing is associated with lowering of testosterone, so it would seem logical to normalise male androgen levels to attempt to maintain biological immortality.
I’m sure that we can all postulate very plausible hypotheses as to why reference ranges are lowering; endocrine disruptors, urine seeping into our water supply from cows pumped full of oestrogen to keep them producing milk(4), ever increasing levels of obesity causing excess aromatisation which exaggerate the negative feedback mechanism of the Hypo-pituitary gonadal system, the list goes on. The fact is, we are so far removed from nature and so deeply entrenched in the machine, we forget that we are biological organisms.
Total testosterone is only part of the diagnostic picture. It is important to factor in the patient’s bioavailable male androgen levels, free testosterone, oestradiol and dihydrotestosterone. Unfortunately, there is no BSSM consensus of opinion regarding normal ranges for these parameters. A level should be considerd supra-physiological when it is associated with either short term and/or long term, negative side effects such as raised blood pressure, raised haematocrit, an abnormal lipid profile and reported gynaecomastia. Supraphysiological levels are not supported by The Men’s Health Clinic as the ultimate purpose of TRT is to help facilitate long term physical and psychological well-being.
Establishing a Diagnosis – Hypogonadism vs Testosterone Deficiency
Testosterone Deficiency can be clinically defined as primary and secondary hypogonadism. There are defined organic pathologies. These are listed in The Men’s Health Clinic TRT Management Guidelines. This page was created as an education tool for both patients and clinicians. The relevant excerpt is below:-
Causes of Primary Hypogonadism:
- Klinefelter Syndrome – A condition in males who have XXY sex chromosomes, rather than the usual XY.
- Bilateral Anorchia – A rare condition in which one or both testes are absent in a phenotypically and genotypically normal male.
- Cryptorchidism – A condition in which one or both of the testes fail to descend from the abdomen into the scrotum.
- Bilateral Orchiectomy – A surgical procedure where both testes are removed.
- Other Organic Aetiology – Trauma / infection to the testes.
Causes of Secondary Hypogonadism:
- Panhypopituitarism – A condition of inadequate or absent production of the anterior pituitary hormones.
- Congenital Hypogonadotropic Hypogonadism – A rare disorder of sexual maturation characterised by gonadotropin deficiency with low sex steroid levels associated with low levels of follicle stimulating hormone and luteinising hormone.
- Constitutional Delay of Puberty – A term describing a temporary delay in the skeletal growth and thus height of a child, with no physical abnormalities causing the delay.
- Hypothalamic or Pituitary Tumour, Destruction or Infiltrative Disease – Such as a pituitary adenoma, traumatic brain injury, pituitary or intracranial surgery, radiation therapy, infection, haematochromatosis.
- Androgenic Anabolic Steroid (AAS) Use – Through suppression of the hypo-pituitary gonadal (HPG) axis from exogenous synthetic testosterone use.
- Hypothyroidism – Causes inhibition of hypothalamic and pituitary production of lutenising hormone.
- Toxins – Medications, illicit drugs, alcohol.
If an organic pathology is not found, the cause of Testosterone Deficiency is likely to be idiopathic; relating to or denoting any disease or condition which arises spontaneously, or for which the cause is unknown. The term Functional Hypogonadism is now well-recognised within the medical community. Some common causes of Functional Hypogonadism can be attributed to past and/or current use of:
- Androgenic Anabolic Steroids
- Alcohol
- Recreational Drugs
- Opiates
- Antidepressants
- Traumatic Brain Injury
Testosterone Replacement Therapy (TRT)
Before considering TRT, it is important that the foundations of health, namely lifestyle, nutrition and physical exercise are addressed. These areas are more specifically discussed in our blog The 10 Testosterone Commandments. It’s also important to look for, and address, any potentially reversible causes. Hypothyroidism is a perfect example of this as an underactive thyroid can have an inhibitory effect on the Hypo-Pituitary Gonadal axis. Conversely, an overactive thyroid can raise Sex Hormone Binding Globulin (SHBG) which will reduce bioavailable male androgen levels. For long term sustainable change, the cause must be addressed, its not a case of simply looking for a solution. There are complexities to this statement, I always talk about the importance of having principles and not rules in medicine, a doctor should always act in the best interests of their patient. Should someone with morbid obesity and low testosterone be told that he’s not a candidate for TRT as weight loss would reduce his propensity to convert testosterone to oestradiol, which in turn lowers his testosterone through negative feedback? The answer is not as clear as you might first think.
If the person sat in front of you is a candidate for TRT based on continued symptoms, diagnostic bloodwork and physical examination, the risks and benefits of engaging in a therapy, that should be considered a lifelong treatment, need to be clearly understood. There should also be a clear understanding of what we are trying to achieve. From a patient perspective, it’s likely a reversal of the negative symptoms and signs associated with having low testosterone, primarily mood, cognitive function, energy and libido. Clinically, I would want the patient to see improvements in all these areas as well, but my focus is actually titrating their male androgen levels to a state where they are working in harmony with the other physiological processes that occur within their body. We should be both working towards their long term physical and psychological well-being, understanding that the journey is complicated by the fact that TRT is not identical to their own natural production of testosterone.
The aim should always be to mimic natural physiology, not enhance it, not alter it, but make it work to promote normality. Testosterone therapy is about replacement, it’s about re-establishing balance within the body.
Gold Standard TRT – Micro-Dosing Testosterone + HCG
My prescribing rationale is clearly explained on The Benefits of TRT page of our website. This page includes links to the relevant research that supports my methodology. Patients are advised that the medications I prescribe are off-label or unlicensed in the UK (but licenced in Europe), and the rationalisation for their intended use. Part of their new patient information pack contains a document explaining this.
The aim of hormone replacement therapy should be to attempt to mimic natural physiology, through replacing the deficient hormones and restoring balance. Homeostasis is a complex mechanism whereby numerous physiological processes attempt to maintain a constant internal environment, despite changes in the external environment. Hormonal stability is fundamental to this process.
By the very nature of injecting a hormone into the body, there must be a rise in the level of that hormone. Through an appreciation of the laws of pharmacokinetics and pharmacodynamics, you can determine the most effective injection frequency and dose. This has been previously addressed in the article Gold Standard TRT, which explains the science behind using small frequent injection intervals to establish hormonal stability. This included a link to ‘The Androgen-Deficient Aging Male: Current Treatment Options‘ demonstrating the resultant hormonal fluctuation associated with using long injection intervals as suggested by the manufacturer.
When monitoring hormone levels, bloods are traditionally measured in a trough, when the level should be at its lowest, just before the next injection. The aim of therapy should be to restore hormone levels and to minimise peaks and troughs. This will help facilitate the body in maintaining this stable internal environment.
Hormones are essentially chemical messengers; they directly influence how their target organs function. Hormonal fluctuations by their very nature must cause a physiological response. According to Bayer Pharmaceuticals, who manufacture Testoviron Depot (Testosterone Enanthate), a single dose of 250mg Testosterone Enanthate leads to a peak (Cmax) testosterone level up to 66nmol/l (19ng/mL) 0.5-5 days post application. They recognise that shorter injection intervals may be needed. They also state that levels returned to pre-treatment levels after two weeks. The laws of pharmacokinetics dictate that more frequent injections lead to more stable levels. If the dose is administered as a single dose of 250mg, this will of course cause supraphysiological testosterone levels within a few days(7), this is something that we are trying to avoid. As stated previously, the rationalisation for micro-dosing is to mimic natural physiology. This helps to achieve stable levels, without peaks and troughs, whilst keeping them within normal physiological parameters. If the normal testosterone reference range is 12-29nmol/l, it is evident that prescribing as per the manufacturing guidelines causes transient supraphysiological levels, with peaks and troughs. This is in opposition to the whole aim of HRT, which is stability.
In other endocrine systems, the dose of the prescribed medication is titrated according to the level of the drug within the body. Blood levels of a drug are influenced by variations in drug absorption and distribution, differences in the body’s ability to metabolize and eliminate the drug, for example genetics; concomitant disease states such as renal or hepatic disease, and physiologic states such as age and obesity; that all have an effect on drug absorption, distribution, and elimination. Within the NHS, this standard does not apply, a fixed dose and injection interval does not allow for biological individuality. This same standard applies to women’s hormone replacement therapy. This one-size-fits-all model does not apply to other endocrine systems such as diabetes and thyroid disorders.
There is a fundamental lack of understanding and appreciation of the role of testosterone within the body due to its association with it use as a Performance Enhancing Drug in sports. Testosterone is an anabolic hormone; its primary role is to help facilitate growth and repair. Anabolic processes predominate at night. Catabolic processes predominate in the day. Testosterone is abused in sports for its anabolic properties. In TRT, it’s use is to simply normalise male androgen levels.
The premise behind hormone replacement therapy should be achieving stable hormonal levels. As discussed, there is a natural diurnal variation in testosterone levels, this can be as much as 20–25% in younger men(8), meaning there is a 24-hour cyclical pattern to male androgen levels. Best practice would be to base your pharmacokinetic – pharmacodynamic model on this physiological process(9).
As stated on The Benefits of TRT page of our website:-
“Micro-dosing is using small volumes of a drug, in this case testosterone and HCG, to achieve more stable levels. It is both safe and effective”.
A recent study ‘Daily subcutaneous testosterone for management of testosterone deficiency’ demonstrated consistent and statistically significant increases in the three testosterone values, total testosterone, free serum testosterone, and direct free testosterone, suggesting that the daily subcutaneous testosterone therapy method used for the patients included in the study has positive effects on testosterone level status. We have also found this in our own clinical practice. Stable levels allow for accurate dose titration allowing me to ensure levels stay within normal physiological parameters.
There is plenty of research to support prescribing outside of manufacturers guidelines to establish more stable levels. This can be evidenced by referring to the following papers:-
- ‘The Androgen-Deficient Aging Male: Current Treatment Options‘
- ‘Pharmacokinetics and Acceptability of Subcutaneous Injection of Testosterone Undecanoate‘
- ‘Pharmacokinetic Profile of Subcutaneous Testosterone Enanthate Delivered via a Novel, Prefilled Single‐Use Autoinjector: A Phase II Study‘
- ‘Pharmacokinetics, safety, and patient acceptability of subcutaneous versus intramuscular testosterone injection for gender-affirming therapy: A pilot study‘
Supraphysiological Testosterone Levels
The aim of TRT is to help restore your male androgen levels to within normal physiological parameters, to reverse the negative symptoms of low testosterone. Whilst it is important to note a qualitative improvement, the clinician’s job is to make sure the quantitative physiological markers remain within the normal range. Whilst testosterone is important for mood, cognitive function and libido, normal levels are necessary for cardiovascular health, bone strength, a healthy lipid profile and red blood cell production.
The BSSM recommends aiming for a total testosterone level of between 15-30 nmol/l when on testosterone replacement therapy (TRT). I have never advocated supra-physiological levels, in fact I actively campaign against them. This is another excerpt from the Benefits of TRT page of our website:-
“Negative health consequences of supraphysiological levels include:
- Decline in mental well-being
- Raised blood pressure & increased cardiac load
- Raised haematocrit
- Abnormal lipid status
- Worsening lower urinary tract symptoms
- Link with prostate cancer
- Gynaecomastia”
I am very prominent on social media, actively campaigning against supraphysiological levels and people advocating testosterone as a lifestyle drug. Testosterone should only be used to correct a confirmed deficiency once possible reversible causes have been addressed. Patients are made aware of a likely titration process as we first need to ascertain how their body is going to respond to treatment, as minor adjustments are made to restore homeostasis. This is partly dependent on whether the patient has more of a primary picture (problem with the testes) or a secondary picture (problem with the brain), however also includes other factors such as Sex Hormone Binding Globulin (SHBG). SHBG acts as a buffer regulating the amount of bioavailable male androgens and fluctuates with varying testosterone levels. This is why regular monitoring is vital and why we insist on six monthly monitoring, rather than twelve monthly as recommended by the BSSM.
Use of Human Chorionic Gonadotropin (HCG)
HCG is routinely prescribed alongside testosterone in America. It forms part of the American Urological Society guidance. We are working very hard to increase awareness surrounding Testosterone Deficiency here in the UK, part of that is highlighting the importance of HCG in TRT. Currently, HCG does not form part of the BSSM guidance. After attending the most recent BSSM conference, I have approached the committee to offer to present the latest research supporting its use alongside testosterone.
HCG mimics Lutenising Hormone (LH)(10). Exogenous testosterone suppresses the release of LH from the pituitary gland resulting in male infertility. LH stimulates the Leydig cells of the testes to produce intra-testicular testosterone. This is then converted to Oestradiol by the aromatase enzyme, which helps support spermatogenesis (sperm production) in the Sertoli cells of the testis. Therefore, HCG is used alongside testosterone to help maintain fertility(11), intra-testicular production of testosterone(12) and testicular size.
HCG is known to help treat male infertility caused by low LH levels(13). A number of NHS Endocrinologists feel “either the patient wants to retain fertility in which case you offer HCG or they do not want to retain fertility in which case you treat with testosterone”. In my opinion, this demonstrates a short-sightedness in her approach to best practice. If testosterone therapy causes male infertility through suppression of LH, the use of HCG to preserve fertility whilst on testosterone should seem like a logical solution to this problem. According to the American Urological Society, the use of HCG alongside testosterone is appropriate to help preserve fertility(14). This recommendation is also supported in other literature(15)(16). In my own clinical practice, we have had nineteen successful pregnancies reported from patients as a direct result of the use of HCG alongside their testosterone therapy, with two of them now having conceived two children.
The premise behind TRT is testosterone replacement, but the premise should be hormone replacement. If we know that exogenous testosterone suppresses LH and that HCG mimics LH, it should seem logical to replace this hormone as standard practice. In addition to the fertility aspect, Testicular atrophy is another common side effect of testosterone monotherapy. The use of HCG alongside testosterone also helps minimise testicular pain and shrinkage.
Subcutaneous vs Intra-Muscular Injections
The Leydig cells produce intra-testicular testosterone in response to stimulation from LH. This unbound Testosterone accounts for approximately 2% of the body’s total testosterone(17). The remaining testosterone is either tightly bound to SHBG, a glycoprotein, or weakly bound to Albumin, another protein produced by the liver. This is because unbound testosterone has a relatively short half-life, between 10-100 minutes. The SHBG and Albumin act as buffers so that the body can regulate the level of bioavailable testosterone within the body. The aromatase enzyme within the testis converts a proportion of testosterone to oestradiol, which helps facilitate the process of spermatogenesis (sperm production) by the Sertoli cells. The remaining unbound testosterone can either be converted to dihydrotestosterone (DHT) by 5-alpha reductase, or further oestradiol in other tissues. It is therefore necessary to have an ester attached to the exogenous testosterone to enable stable levels. The longer the ester, the longer it takes for the testosterone to be released.
Testosterone preparations needs to enter the venous system to be transferred to the liver in order to have the attached ester cleaved. Testosterone has traditionally been administered via the intramuscular route as it is highly vascular. If the ester is cleaved too quickly, there can be a spike of oestradiol which can cause negative side effects such as anxiety, water retention, bloating and potentially gynaecomastia (breast tissue). The subcutaneous route is a suitable alternative as the absorption is delayed. Oil injected into this area encounters adipose (fat cells), collagen and fibrous tissue before entering capillaries, which then form veins and the lymphatic system, eventually joining the venous system(18). This essentially dilutes the rate of absorption, which not only leads to stable levels(19), but also less aromatisation of testosterone to oestradiol. Injecting into the subcutaneous space is also less painful and better tolerated than injecting into the muscle(20).
Gold Standard TRT – Daily Subcutaneous Injections of Testosterone Cypionate & HCG
Safety should always be of paramount importance in any medical field, but the regressive culture displayed within the medical community is causing dissatisfaction and potential harm.
“Hypogonadism is misdiagnosed, over-diagnosed and undiagnosed in equal measures.” – Society for Endocrinology Position Statement on Male Hypogonadism and Ageing
This has led to the emergence of ‘providers’ who are promoting TRT as a lifestyle drug and advocating remote prescribing despite the GMC advice to the contrary when dealing with complex medical conditions(21). NHS Endocrinologists are understandably becoming more concerned with irresponsible over-prescribing and poor prescribing habits. Such practice can cause additional unnecessary workload on an already overstretched, under-resourced NHS. The emergence of ‘providers’ should be the necessary prompt for them to address the shortcomings that are evident in their current medical model, rather than adopting a blanket resistance to change due to the misassociation of all non-NHS practice being unsafe. It should prompt them to look to a more progressive model that focuses on the best interests of the patient.
I am pleased to report however that the tide is beginning to turn, and attitudes are slowly changing. In the past three months we have received two referrals from NHS GPs, as well as a private referral from a Professor of Endocrinology. The Professor of Endocrinology is already aware of, and supports, my work. We have also been advised of a possible imminent referral from an NHS Endocrinologist.
In addition to this, we have recently been informed by one of our patients that the NHS, on the advice of his NHS Endocrinologist, will support him in prescribing both his testosterone and HCG, in addition to performing the necessary blood tests on the NHS, whilst remaining under our care and supervision at The Men’s Health Clinic.
I am open and transparent about my prescribing rationale because I want to make what is considered “very unconventional” by some NHS Endocrinologists, standard practice in the future. The opinion that the term “gold standard” is misleading is simply not the case ,as the research and our patient outcomes demonstrate the assertion. We have recently been inspected by the CQC who deemed our service ‘Good’ in all 5 of the key standards with no recommendations for improvement. A copy of the report can be found here. Our patient testimonials speak for themselves when questioning whether patients value GOLD STANDARD care.
“The goal of Testosterone Replacement Therapy is normalisation of male androgen levels to within normal physiological parameters for long term physical and psychological well-being. It is not about gym muscles; it’s about achieving normality and reversal of the negative symptoms associated with Testosterone Deficiency.”
Dr Robert Stevens MBChB MRCGP Dip.FIPT


