Alcohol, Sex Hormones & Cardiometabolic Health

Alcohol is entangled with our modern human history. We’ve enjoyed a 9,000-year love affair with it, with evidence pointing to our consumption of alcohol dating back to as early as 6000 to 4000 b.c. 1. It’ has shaped our culture from the very start, and many of you reading this have likely consumed alcohol at least once in your life, if not weekly or daily. However since the start, we’ve also known that detrimental effects of excessive drinking existed too, the most notable being alcohol poisoning and behavioural changes from being too drunk.
Our understanding of alcohol’s effects on the body has improved drastically with modern science. It’s clear that there’s a mix of effects, and public health officials know this. But this blog is writing for a case to exclusively abstain from drinking, on the contrary, letting loose sometimes can help with one’s mental health. However, moderation and balance are key components to many things, and alcohol is included in that. It’s something best served in small doses. Regardless, this blog will focus on informing you of a measured account of both the potential positive and detrimental effects of excessive drinking, specifically relating to your sex hormones and general metabolic health. This will all be based on the science.
It’s important to mention that alcoholism is a big health issue. If you do drink too much (understandably during these stressful times), it’s important for you to review ways to reduce it and seek help if you struggle. This can be very bothersome and difficult, but to quote Plato, “Attention to health is life’s greatest hindrance”. Sometimes you must cut back on your indulgence in certain things to be healthy, which is imperative to living a long-lasting life, and helps address some aspects of mental health too.
Alcohol & Cardiometabolic Health
Alcohol is complicated, it has both potential benefits and known risks. For example, epidemiologic studies have documented that moderate alcohol intake, versus abstinence, can lower the risk for coronary heart disease (CHD) 2. But, don’t raise your glass in celebration just yet. These associations are between moderate drinking, and don’t necessarily mean that alcohol is the cause of the lower risk. Reviewing the populations used in the studies it becomes apparent that perhaps alcohol abstainers had greater mortality rates due to socioeconomic and employment status, mental health, overall health, and other health habits such as smoking 3.
High consumption of alcohol has in fact been shown to increase the risk of death from other types of heart disease, in addition to cancer, liver cirrhosis, and trauma 2. This is consistent in literature, even in more recent reviews where some argue that even light alcohol consumption is bad 4.
Don’t dump the beer, wine, gin etc. so fast though, recall I said that alcohol is complicated and science rapidly evolves. So, let’s break it down using large-scale studies and focus on cardiometabolic health.
Before we move on, for reference one unit of alcohol in the UK is about 8 grams of pure alcohol. A glass of wine at 12.5% volume will contain 10g of alcohol per 100 ml of wine; the same as 1 drinking unit. The figure below from NHS Grampian gives a very good visual guide to units and your drink.
Figure 1 – What’s a unit of Alcohol? 5 (click for full-size image)
Hypertension
In women, heavy alcohol consumption is linked to hypertension. Consuming 20-34 grams of alcohol per day (2.5 to 4.25 units), versus 0g/day, demonstrates a strong link. However, when we examine the impact as part of a healthy lifestyle among middle-aged women, the incidence of hypertension is lowest among those drinking 0.1 to 5.0 grams per day (<1 unit) or 5.1 to 10.0 grams per day (<1 to 1.25 units) 6. This could be in part due to alcohols positive impact on endothelial (blood vessel) function in small doses, but high daily levels and binge drinking may well impair it. The mechanism by which this occurs is interesting, but beyond the scope of this blog. So, one unit of wine per day keeps hypertension at bay in women.
In men there appears to be a more pronounced linear increased risk for hypertension as alcohol consumption increases. The risk still exists, even with alcohol intake less than 10g/day 7, but before assuming alcohol is sexist and start writing a long defensive wall of text, there may be more to consider. Men typically engage in riskier behaviour, which may already increase their risk for elevated hypertension 8. In addition to this, there may be other compounding factors that affect these results. This includes lifestyle and other dietary habits, i.e. being sedentary, overweight/obese and eating high calorie, high-salt diets. Regardless, based on the data, it’s recommended that men limit their alcohol consumption to no more than two units per day, and women to no more than 1 unit per day (sorry, Lydia) 7.
Coronary Heart Disease (CHD)
Comprehensive systematic reviews and meta analyses have shown that alcohol consumption between 2.5 g/day and 30 to 60 g/day (<1 unit/day to ~5 unit/day) are cardioprotective. Consume more than this and we run into problems. Furthermore, those who are of South Asian ethnicity in the INTERHEART study appeared to not get this cardioprotective effect. This is perhaps related to a genetically increased risk for cardiovascular disease and diabetes among South Asian populations 7.
Stroke
There appears to be a J-shaped relationship with alcohol intake and stroke; that is 0 to 20 g/day (< 2 units) appears to reduce the risk of stroke. Greater than this and we see an increased risk.
However, further studies only seem to demonstrate this protective effect if you carry a certain variant in the alcohol dehydrogenase ADH1B gene (rs1229984). The protein encoded by this gene plays a big role in metabolising ethanol (alcohol). It has been identified that individuals with the A allele mutant (a single base change, which is a mutant gene in layman terms) that consume low-to-moderate alcohol will see beneficial cardiovascular health outcomes 7. This is incredibly important to note as it suggests that traditional studies may not capture important nuances that cause bias. Which brings me back to saying that alcohol is complicated. I’ll add to this by saying that studying it is multifactorial and complex too. Its effects may be more or less beneficial depending on your genetic makeup and, short of paying for a ~£140 test, you likely won’t know your genetic risk factor, so don’t worry.
Diabetes Mellitus
Alcohol quite easily contributes to obesity via excess caloric intake; 1 gram of alcohol is ~7kcals, which does not include additional calories in the beverage from carbohydrates, i.e. the various sugars in your mixers and cocktails. Obesity is also well linked with type 2 diabetes mellitus (T2DM).
Alcohol in heavy quantities is known to have a direct diabetogenic effect, greatly disturbing carbohydrate and glucose metabolism and also impairing liver function 9. Several studies have noted that there is a significantly increased risk of T2DM with high alcohol consumption. However, in moderate consumption (17 grams, or about 2.12 units per day) it lowers the risk in women, but increases it in men 10,11. It has been postulated that the gender differences could be due to the impact that alcohol has on sex hormones; in men it lowers testosterone. We’ll dig that hole a bit more in the next section.
Visceral Fat
Visceral fat is intra-abdominal fat, located inside the abdominal cavity and packed between organs. Excess visceral fat is known as central obesity, which more often affects men and menopausal women due to sex hormone differences.
It is well known that excess alcohol can encourage a beer belly, a byproduct of increased visceral fat. Many iron-liver beer champions can attest to this with their mighty beer bellies. Additionally, alcohol consumption greater than 14 units per week (2 units/day), is associated with an increased risk of metabolic syndrome 12,13. Even with light-to-moderate drinking, we don’t see a protective effect on visceral adipose tissue accumulation. If you’re getting enough calorific energy from your diet, it will pack on visceral fat. The more alcohol or calories, the more visceral fat.
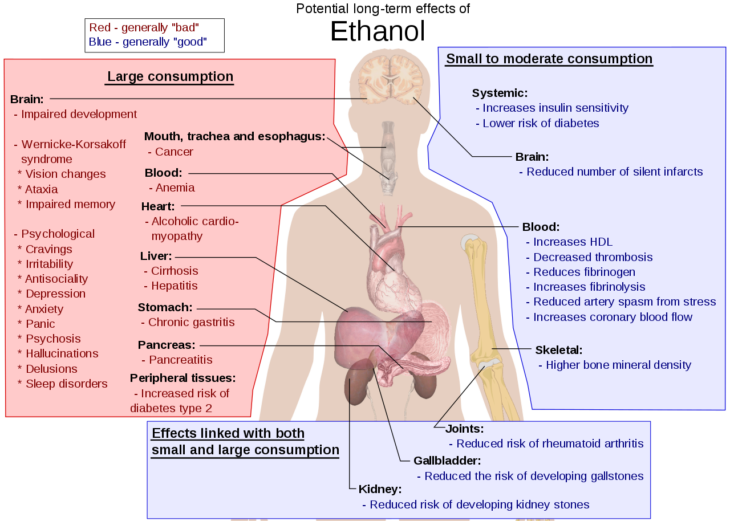
I can continue with talking about the negative and positive cardiometabolic effects of alcohol, including the known fact that alcohol is well linked to liver diseases 14. I could even talk about other non-communicable diseases, but unfortunately there isn’t enough space to write about it. Instead, take a look at the figure below for an overview of some positive and negative effects of alcohol in long term consumption.
Figure 2 – Potential long term-effects of alcohol consumption 15 (click for full-size image)
We need to consider that not every study controls for lifestyle, exercise frequency, diet, age, ethnicity, genetics, stress levels, and socioeconomic status. These are all important factors that contribute to cardiometabolic diseases and alter our risk accordingly when consuming alcohol.
Alcohol, Aromatase & The HPG Axis
Something that’s often observed in chronic drinkers is a marked reduction in Testosterone, concurrent with an increase in plasma oestradiol 16. It’s in-fact plausible that the cardioprotective effects and reduced risk of osteoporosis associated with low dose alcohol consumption could in part be due to the elevation in oestrogen, at least in women. This correlates well with the fact that we see an increased risk of breast cancer among female drinkers too.
But why does this occur? In male rats, heavy alcohol consumption leads to increased aromatisation of androgens in the liver 16. This is consistent in animal models, going as far to consider high alcohol consumption to be a chemical form of castration 17. Is this a by-product of impaired liver function? Okay, you’re not a rat, but it affects human alcoholics just the same; we see significantly increased FSH, LH, and oestrogen levels, with a concurrent decrease in testosterone and progesterone including alcoholic patients without cirrhosis 18. This problem is worsened in those with liver disorders. Why? Because the liver is a prime site of aromatase expression.
Diseased liver states such as hepatitis and hepatocellular carcinoma, also see increased aromatase expression and elevated oestrogen 19. Alcohol, more so Ethanol, increases aromatase activity in the liver. Furthermore, alcohol causes a decrease in IGF-1 bioavaibility due to altered liver function. This may contribute to the development of hypogonadism as IGF-1 is known to stimulate testosterone synthesis in animal models 20,21. Another warning: this adversely affects the circadian rhythm, which is important. You will know this if you read my blog on the endocrine system and sleep.
I’m sure you’re aware by now that elevated oestrogen will naturally lead to decreased testosterone. This is due to negative feedback of the hypothalamic–pituitary–gonadal axis (HPGA), described in the figure below.
Figure 3 – HPGA feedback loop 22 (click for full-size image)
What occurs is alcohol induced hypogonadism. But the question is, in what dose? How much alcohol is bad? Most studies suggest that it’s moderate-to-high consumption that is problematic. The recommendation of <14 units per week for men probably holds quite true for those who want to maintain optimal health. Also, don’t think you can escape this issue if you’re on TRT; too much alcohol will result in elevated oestrogen and decreased IGF-1, impairing fertility in addition to general health. If you are on HCG, alcohol may well negatively affect testosterone synthesis from HCG too. Don’t forget the general negative health effects of alcohol too, including increased liver strain. Keep to the advice and stick to less than 14 units a week. Don’t binge either, binge drinking can be just as, if not more, harmful to your health.
Concluding Remarks
Alcohol is incredibly good at making us relax and forget our stress and anxieties. But, it’s a double-edged sword. It can lead to worse-off health which, in turn, worsens our stress and anxieties, as well as shortening our lifespan. Furthermore, chronic moderate-to-high consumption will raise oestradiol (and significantly lower testosterone for those not on TRT). Is this to say that you can’t or shouldn’t drink? No, moderation is key, just limit yourself to what is recommended. Don’t binge and don’t drink excessively, no matter how strong your liver is. Drinking excessively to the point of drunkenness on a consistent basis is unhealthy, no matter what. If you are suffering with this, I would encourage you to try to identify what is causing you to drink, and address this. Turn to support groups if you are struggling, for both your health and the health of others. Drink responsibly, exercise, eat well, meditate, enjoy life and stay healthy.
References
- Our 9,000-Year Love Affair With Booze. https://www.nationalgeographic.com/magazine/2017/02/alcohol-discovery-addiction-booze-human-culture/. Accessed June 20, 2020.
- Health risks and benefits of alcohol consumption. Alcohol Res Heal. 2000;24(1):5-11.
- Fillmore KM, Golding JM, Graves KL, et al. Alcohol consumption and mortality. I. Characteristics of drinking groups. Addiction. 1998;93(2):183-203. doi:10.1046/j.1360-0443.1998.9321834.x
- Tahan AC, Tahan V. Alcohol is not safe even at light amounts. Balkan Med J. 2015;32(2):239. doi:10.5152/balkanmedj.2015.150853
- Grampian N. What is a unit of ALCOHOL? http://www.nhsgrampian.org/nhsgrampian/gra_display_simple_index.jsp;jsessionid=370F9902C1B69A5272FB6A963BDB1C0F?pContentID=7493&p_applic=CCC&p_service=Content.show&.
- Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB. Key findings on alcohol consumption and a variety of health outcomes from the nurses’ health study. Am J Public Health. 2016;106(9):1586-1591. doi:10.2105/AJPH.2016.303336
- Piano MR. Alcohol’s Effects on the Cardiovascular System. Alcohol Res. 2017;38(2):219-241. /pmc/articles/PMC5513687/?report=abstract. Accessed June 20, 2020.
- Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography Soc Biol. 2015;61(1):1-17. doi:10.1080/19485565.2014.929488
- Kim SJ, Kim DJ. Alcoholism and diabetes mellitus. Diabetes Metab J. 2012;36(2):108-115. doi:10.4093/dmj.2012.36.2.108
- van Dam RM. Alcohol consumption and risk of type 2 diabetes in east Asian populations: Do healthy patterns of consumption exist? J Epidemiol. 2018;28(3):106-107. doi:10.2188/jea.JE20170151
- Crandall JP, Polsky S, Howard AA, et al. Alcohol consumption and diabetes risk in the Diabetes Prevention Program. Am J Clin Nutr. 2009;90(3):595-601. doi:10.3945/ajcn.2008.27382
- Kim KH, Oh SW, Kwon H, Park JH, Choi H, Cho B. Alcohol consumption and its relation to visceral and subcutaneous adipose tissues in healthy male Koreans. Ann Nutr Metab. 2012;60(1):52-61. doi:10.1159/000334710
- Lemos-Santos MGF, Valente JG, Gonçalves-Silva RM V, Sichieri R. Waist circumference and waist-to-hip ratio as predictors of serum concentration of lipids in Brazilian men. Nutrition. 2004;20(10):857-862. doi:10.1016/j.nut.2004.06.005
- Frazier TH, Mcclain CJ, Kershner NA, Marsano LS. Treatment of alcoholic liver disease. Therap Adv Gastroenterol. 2011;4(1):63-81. doi:10.1177/1756283X10378925
- Mikael Häggström. Potential long term-effects of alcohol consumption. https://en.wikipedia.org/wiki/Long-term_effects_of_alcohol#/media/File:Possible_long-term_effects_of_ethanol.svg.
- Purohit V. Can alcohol promote aromatization of androgens to estrogens? A review. Alcohol. 2000;22(3):123-127. doi:10.1016/S0741-8329(00)00124-5
- Kyung Won Chung. Effects of chronic ethanol intake on aromatization of androgens and concentration of estrogen and androgen receptors in rat liver. Toxicology. 1990;62(3):285-295. doi:10.1016/0300-483X(90)90052-I
- Martínez-Riera A, Santolaria-Fernández F, Gonzalez Reimers E, et al. Alcoholic hypogonadism: Hormonal response to clomiphene. Alcohol. 1995;12(6):581-587. doi:10.1016/0741-8329(95)02006-3
- Hata S, Miki Y, Saito R, Ishida K, Watanabe M, Sasano H. Aromatase in human liver and its diseases. Cancer Med. 2013;2(3):305-315. doi:10.1002/cam4.85
- Castilla-Cortazar I, Quiroga J, Prieto J. Insulin-like growth factor-I, liver function, and hypogonadism in rats with experimentally induced cirrhosis [1]. Hepatology. 2000;31(6):1379. doi:10.1053/jhep.2000.7886
- Roser JF. Regulation of testicular function in the stallion: An intricate network of endocrine, paracrine and autocrine systems. Anim Reprod Sci. 2008;107(3-4):179-196. doi:10.1016/j.anireprosci.2008.05.004
- Michael Scally. Hypothalamic Pituitary Testes Axis. http://www.asih.net/hpta.htm.