A Guide To Steroid Hormones & Immunity
Amid this awful viral pandemic, global economic meltdown and toilet paper shortage, you may be worried about how your TRT might influence your immune system. Well, don’t panic because I’m going to explain this to you in this article.
Glucocorticoids, Sex Hormones & Immunity – Definitions
Glucocorticoids are steroid hormones, named rightly so as a portmanteau (glucose, cortex, and steroid) that’s involved in the regulation of glucose metabolism, is synthesised in the adrenal cortex of the kidneys, and is steroidal in structure. Cortisol is a glucocorticoid. Glucocorticoids also play an important role in the immune system, alertness, cognition, and body fluid homeostasis. But these are just a few of the important thing’s glucocorticoids do. Contrary to typical ‘bro-science’ advice, glucocorticoids are essential to your wellbeing and are in tight homeostatic control with sex steroid hormones. Yes, that includes cortisol.
Sex-steroid hormones (also known as gonadocorticoids), such as Androgens (i.e. Testosterone) and Oestrogens (i.e. Oestradiol), regulate diverse physiological functions, including reproduction, the immune system, sexual arousal, maintenance of secondary sexual characteristics (such as pubic and facial hair in men), response to stress, cognition, and various metabolic processes (Tatiana, 2012).
Your immune system is the defence system that’s composed of various organs and processes which provide resistance to infections and toxins. It has many layers to it. It helps keep germs (pathogens) like bacteria, viruses, fungi and parasites out. The immune system is indeed a complicated system and a whole field of study has been dedicated to it, named immunology.
By now you’re probably aware that infections spread through different means, some via breathing in droplets from someone else’s sneeze or cough, having unprotected sex, via bodily fluids, and touching any contaminated surface. But have you ever wondered what your immune system is and what makes it tick? Let’s first examine what interactions glucocorticoids and sex hormones have with the immune system.
The Immune System Has Many Layers – A Basic Guide to Those Interested in How the Immune System Works
This section may be a bit difficult to understand, so feel free to skip it. But note that it will help you understand the role of steroid hormones in the immune system a bit better. It’ll also help you learn a bit about the awesome infection and injury fighting army that’s inside your body.
There are primarily three defences against infection; the innate immune system, nonspecific responses to infection, and the adaptive defence system.
The Innate Defence – The First Line of Defence
This line of defence is composed of physical or mechanical barriers and chemical defences.
Physical or Mechanical Barriers
- The Skin – The skin acts are a barrier to stop infection from entering your body, and sebaceous glands in the skin produce sweat and sebum, which contain antiseptic molecules that can break down bacterial cell walls and help further protect the skin. Additionally, the skin contains nonspecific inhibitors which act to inhibit viruses and bacteria. But the skin isn’t perfect and can become infected.
- Mucus Membranes – Another important line of defence that lines body cavities exposed to the world, including nostrils, the lips, ears, the genital area, and anus. Particularly in the respiratory tract, mucus helps trap bacteria and foreign debris, which can then be cleared up by immune cells. Some mucous membranes are ciliated, meaning they contain tail-like projections that extend outside the cell body and move the mucous across the surface.
Chemical Defences
- Tears and Saliva – Both contain lysozyme, which is an antiseptic enzyme that can attack the cell walls of bacteria and break them down
- Stomach Acids – Glands inside your stomach lining produce hydrochloric acid, which kills most organisms that you swallow.
- Urine in the Urinary Tract – Helps prevent multiplying of harmful organisms in the genital tract area.
Nonspecific Responses to Infection – The Second Line of Defence
These nonspecific responses include both the physical and chemical barriers, inflammatory responses, and interferons (Gooch, 2011). The nonspecific defences will act sooner than specific defences (which will be discussed shortly). Some, are always present, including barriers, nonspecific inhibitors (body fluids containing viral inhibitors, such as certain lipids, proteins, lipoproteins, glycoproteins, and polysaccharides/certain carbohydrates), and phagocytic cells (white blood cells – polymorphonuclear leukocytes and macrophages that ‘eat’ the viruses). Others are evoked by infection (fever, inflammation, and interferons).
Inflammatory Response
A break in the skin, i.e. caused by a cut, will allow foreign pathogens into the body. This will cause swelling (tumor), heat (calor), reddening (rubor), and often pain (dolor) at the site of injury. This is an inflammatory response.
Why? When injuring the tissue, several cells rupture and release histamine and kinins, which are chemicals that make the capillaries dilate (expand), become more permeable (liquids or gasses pass through easier), and leak fluid into the tissue. This causes the swelling, redness, and heat. The swelling and kinins stimulate nerve endings and kinin receptors to cause pain. Acid production also occurs, which is unfavourable conditions for pathogens.
Why would the body do this? Because it can help inhibit viral replication via elevating the local temperature (pathogens operate best at certain temperatures), increase acid production, reduce oxygen tension (less oxygen for pathogens), alter the metabolism, and increase acid production.
Neutrophils, monocytes, and macrophages may also be attracted and attempt to ‘eat’ the invading pathogens. As phagocytosis is receptor mediated (i.e. it’ll only bind to receptors that aren’t its own) it ensures only pathogens are ingested.
Complement System
The complement system simply enhances the ability of antibodies (Y shaped protein that helps neutralize pathogens) and phagocytic cells to clear microbes and damaged cells and it also promotes inflammation. It has many small plasma proteins that work together to ultimately cause death of the invader. It looks a bit like this (click for full-size image):
The complement protein here is called the Membrane Attack Complex, which is a circular membrane that attacks the cell membrane of the pathogen and forces cytoplasm (fluid inside the pathogen) to rush out, and fluids to rush in, causing the pathogen to rupture and die, or be defunct (Bayly-Jones et al., 2017).
Interferons
Interferons (IFNs) are glycoproteins (glycogen attached to proteins) which interfere with viral growth, and enhance the killing ability of granulocytes, macrophages, natural killer cells, and cytotoxic lymphocytes.
How does this come to be? Well, when a cell has been infected by a virus, it hijacks the cells replication mechanism to make viral nucleic acid (makes copies of itself), but this is used as a signal for the cell to realize it’s infected. The cell then creates and sends INFs outside, which warns nearby healthy cells too. In response, the healthy cells also make changes to defend themselves to a virus (Gooch, 2011).
Adaptative Defence – The Third & Final Line of Defence
In this pathogenic war, there is a final wall of defence. The part of the immune system that will directly target and hunt down the invaders. This specific immune defence responds to antigens.
Antigens are proteins, or polysaccharide molecules which are typically found on the cell membrane (the body recognizes its own, called nonself). They’re also found on pathogens, foreign cells, and cancer cells (not nonself).
Recall I mentioned some white blood cells, including lymphocytes? They play a big role here.
Lymphocytes
There are 2 types of the small white blood cell called a lymphocyte. A B cell and a T cell. Both cells can recognize target cells carrying antigens but do this in different ways.
B Cells
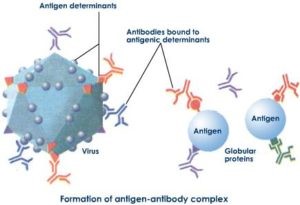
B cell lymphocytes are primarily responsible for the body’s antibody mediated immunity; they create antibodies. Antibodies are Y shaped proteins that’ll bind with the foreign antigens and neutralize them. To put simply, they act as a marker for destruction and they immobilize the virus. They can also neutralize toxins.
If you were to imagine it, it’d be a bit like this (click for full-size image):
There are variations of B cells, including memory B cells which are long lived and contain the antibodies against an antigen so they can be created much faster, should a second exposure occur. In-fact, during second exposures, we tend to produce many more antibodies, hence why we often receive booster shots for certain diseases.
T Cells
T lymphocytes carry out something called cell-mediated immunity (CMI). When a macrophage phagocytizes (eats) the invader, it presents the invaders antigens to a T cell lymphocyte. This turns on the appropriate T cell, which rapidly multiples to form cytotoxic T cells (Tc cells), and these cells will travel to the site of infection and produce chemicals (perforins – which cause pores to form in the membrane of the target cells, causing it to burst, known as lysis) to kill the invaders.
Some of these activated T cells become memory T cells (Tm) which will recognise the foreign antigens and thus respond quicker should a second exposure occur. There are other T cells, but this goes beyond the scope of what we need to know here.
Glucocorticoids, Sex Hormones & Immunity – Interactions
I do further describe the immune system at a high (but relatively basic) level in the last section. It’s not essential to read but may help clear up any things you don’t understand. In this section, I don’t want to list each interaction the hormones have with the immune system, as this merely aims to give you an overview.
Both glucocorticoids and sex steroid hormones will affect the function of various innate immunity cells. This includes neutrophils, macrophages, and natural killer cells. To concisely summarise the differing effects, glucocorticoids mainly supress the cells of innate immunity (Bereshchenko et al., 2018). They also suppress the inflammatory response we often see. This explains why you may be given a ‘steroid’ shot after getting a bad injury.
Now, before you think that glucocorticoids are good because they’re anti-inflammatory – there are situations where we want inflammation, such as after an injury or infection. In the short run, it will help mobilize the responses we need to fight said infection. However, chronic inflammation can be bad. Therefore, glucocorticoids are necessary; to exert anti-inflammatory effects and balance the immune responses.
As one may expect, the effects of glucocorticoids and sex steroid hormones differ. Generally, though, Testosterone exerts suppressive and modulatory effects on both the humoral and cellular immune Reponses and thus acts to be anti-inflammatory in nature. Oestradiol instead exerts immunoenhancing activities on the humoral immune response (Cutolo et al., 2002). Please don’t assume that Testosterone therefore increases the risk of infection; you produce Oestradiol too, which helps enhance your immune response.
Chronic inflammation can lead to diseases like Rheumatoid Arthritis (RA) and is often seen in other diseases such as Type 2 Diabetes Mellitus. It’s no surprise that the body fluid of RA patients tends to be low in sex hormones (Cutolo et al., 2002). Sex hormone balance is a very crucial factor in regulating your immune and inflammatory responses.
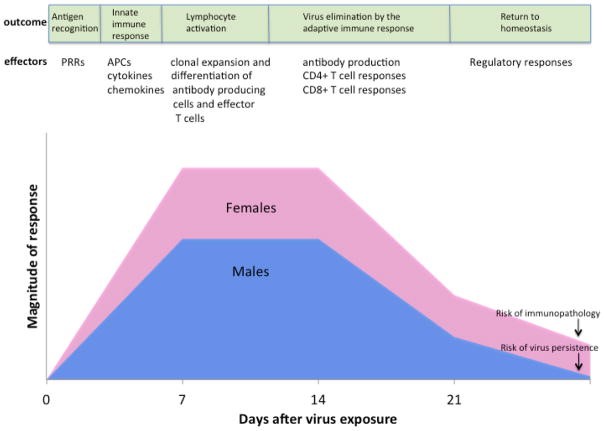
Generally, in women we see a much bigger immune response following viral exposure. This may well be due to oestradiol’s immunoenhancing effect, which leads to an increased risk of immunopathology (i.e. tissue damage by high or prolonged activation of immune response) when returning to a normal, non-infected state. Men contrastingly have a lower magnitude of response, but risk persistence, including viral persistence (the pathogen isn’t fully cleared from the body and infection may last longer), this is well characterised in the graph below (Klein, 2012) (click for full-size image).
Still, as it’s topical, you’ll be pleased to know that Oestradiol is indeed protective against Influenzas (flu), due to increasing Neutrophil count and virus-specific cytotoxic T cell responses in the lungs (Robinson et al., 2014). Additionally, low levels of testosterone, which lead to low levels of oestradiol, lead to increased rates of infection (Nakashima et al., 2017). Why? One reason is this delicate balance of regulating the immune system and inflammatory responses, alongside glucocorticoids. There’s also the possibility that increased muscle mass leads to higher plasma gelsolin; a protein which has antimicrobial actions. Conversely, supraphysiological levels of testosterone are very likely immunosuppressive and can lead to an increased risk of infection (Trumble et al., 2016).
So, to summarise – TRT will not increase your risk of infections. Low Testosterone and Oestradiol, likewise supraphysiological levels, can. As can improper glucocorticoid levels. How does this fit in with coronavirus? It’s likely that TRT will be protective against COVID-19 due to the mechanism by how COVID-19 infects cells and Testosterones regulatory effects on ACE2 receptors.
However, we can’t say much with certainty as the data present has so many uncontrolled factors and it won’t change the fact that if you aren’t maintaining good hygiene and social distancing during a global pandemic, you may well get COVID-19 no matter what.
Viruses, Coronaviruses, Bacteria, Fungi & Parasites – What Are They?
I’ve included this section for those of you who are interested in knowing the basic differences between each of the foreign invaders your body may have to fight off.
What’s a Virus?
A virus is a non-living, infectious agent that is composed of protein and nucleic acid (organic substance often found in DNA or RNA). It can reproduce by invading and hijacking a cells replication machinery, as they lack their own for self-replication. You’ve likely encountered many in your life, including influenza and the common cold (rhinovirus and coronaviruses). Some are more deadly than others, such as HIV, and certain other viral strains (i.e. MERs or SARS-CoV-2, which causes COVID19). Provided you’re otherwise healthy, your immune system will have done its job in fighting these viral invaders throughout your life, in addition to killing off your body’s own bad and cancerous cells, every single day.
You can help prevent catching or spreading a virus by coughing and/or sneezing in tissues and disposing of them and then washing your hands properly with hot water and soap for at least 20 seconds. Do also avoid those with viral infections; the last thing you want to do is pick it up and pass it onto someone less able to fight it off. Antiviral drugs can treat certain viral infections.
What is Coronavirus?
Coronaviruses are a group of related viruses which cause respiratory tract infections, in humans. They can be mild, such as those causing the common cold (predominantly caused by rhinoviruses), whereas others can be lethal, such as SARS-CoV, MERS, and SARS-CoV-2 which causes COVID-19 (yes, the virus that makes people buy toilet paper).
As it is mandatory to say during a pandemic, COVID-19 is indeed dangerous. I won’t detail why COVID-19 is dangerous, but as someone who is working on research with it, please let me be very clear. It’s not just a ‘flu’, it can be fatal to those venerable and even some young people. Wash your hands with hot water and soap for 20 seconds, stay at home, keep your social distance, and if you have any symptoms, self-isolate immediately. Please also stop panic buying and do help your community.
What are Bacteria, Fungi & Parasites?
Bacteria are single celled organisms that can live in diverse environments. Not all bacteria are bad, we have some that help with digestion and prevent bad strains from growing. They play an important role in the nutrient cycle too, in addition to the decomposition of dead bodies; they are essential to our survival. We also can genetically engineer bacteria to produce drugs.
Irrespective, pathogenic bacterial infections can cause a range of issues, and can be transmitted via different routes. This includes poorly prepared food (lending to food poisoning i.e. via E.coli or Salmonella), from touching contaminated surfaces, via bodily fluid, and sexual transmission. For most bacterial infections, we can treat them with antibiotics, which can either kill bacteria or inhibit its growth. Our immune system will also fight these pathogens.
Fungi is any member of the eukaryotic (cells which have a nucleus –where you’ll find the DNA/RNA) organisms, including microorganisms such as yeast and moulds, in addition to mushrooms. They also play an important role in our ecosystem, and in making alcohol. However, certain fungi can cause mycosis (fungal infection). They can be picked up from fungal spores, i.e. from mouldy food, or inhaling nearby fungal spores. Topical and systemic antifungal drugs can be used to treat mycoses.
Parasites, in humans, include protozoa (single-celled eukaryotes) and worms. One example is Malaria, which is transmitted via mosquitos. Another is Leishmaniasis which is spread by the bites of certain sand-flies (WHO, 2020). Some parasites can also be transmitted by poorly cooked food.
Maintaining good hygiene behaviours (including food hygiene), keeping vaccinated, keeping healthy by exercising and having a good diet, taking preventive medication where needed, and avoiding high-risk areas, will help prevent you being infected by any of these things.
Key Points & Important Links
Below are the key points to take from this article, and important links to refer to regarding the current Coronavirus pandemic.
- Testosterone can be immunosuppressant, mostly anti-inflammatory, as well as immunomodulatory.
- Oestrogens are immunoenhancing, mostly anti-inflammatory, as well as immunomodulatory.
- Glucocorticoids are highly immunosuppressant and anti-inflammatory.
- These hormones all work together to help you fight infections and recover from injuries. But the balance of these hormones is key to ensuring we don’t have an over or under responsive immune system.
- We must aim to be within physiological ranges of these hormones, and at a level that’s optimal for you, to also have a healthy immune system.
- You need to also take good care of yourself by means of exercise and diet to further improve your immune system responses.
It doesn’t matter if you feel like Superman on TRT, or your vitamin C makes you feel great, you are NOT invincible. You can decrease you risk of infecting yourself or others by doing the following:
- Washing your hands often
- Getting vaccinated
- Using antibiotics sensibly (when prescribed and continue the FULL duration)
- Being smart about preparing food (keep surfaces clean, promptly refrigerate leftovers, and cook food properly).
- Disinfect ‘hot zones’ where you reside, including the kitchen and bathroom
- Practice safer sex using condoms and get tested for STDs
- Don’t share personal items, including toothbrushes, combs, and razor blades. Avoid sharing drinking glasses or dining utensils.
- Travel wisely – try not to travel when ill, as you can affect nearby passengers.
- Socially distance or isolate yourself if ill. Though I appreciate there may be economic difficulties with this, it is important.
For details about Coronavirus symptoms and risk factors, please go to the following links:
Main Keywords:
- Innate Immune System – The first line of defence in the immune system that’s nonspecific to a disease.
- Inflammation – Response to harmful stimuli, i.e. from pathogens, damaged cells, or irritants. Leads to heat, swelling, redness, and pain.
- Immunosuppressant – Supresses the immune system
- Immunoenhancer – Increases immune system response
- Chronic – Persistent illness
- Acute – Abrupt onset of disease that’s generally short duration and rapidly progressive (in need of urgent care)
Wrap Up
To reiterate, a healthy balance of physiologically normal and balanced hormones leads to a good immune response that’s well balanced. But it doesn’t change the fact that you need to follow the given advice. Be hygienic and think first when you’re ill; don’t spread it. I hope this article helps put your fears to rest. Make sure you exercise during this lockdown, try your best to eat well, and keep in touch with loved ones.
References
- Bayly-Jones, C., Bubeck, D., & Dunstone, M. A. (2017). The mystery behind membrane insertion: A review of the complement membrane attack complex. In Philosophical Transactions of the Royal Society B: Biological Sciences (Vol. 372, Issue 1726). Royal Society. https://doi.org/10.1098/rstb.2016.0221
- Bereshchenko, O., Bruscoli, S., & Riccardi, C. (2018). Glucocorticoids, sex hormones, and immunity. In Frontiers in Immunology (Vol. 9, Issue JUN). Frontiers Media S.A. https://doi.org/10.3389/fimmu.2018.01332
- Cutolo, M., Seriolo, B., Villaggio, B., Pizzorni, C., Craviotto, C., & Sulli, A. (2002). Androgens and estrogens modulate the immune and inflammatory responses in rheumatoid arthritis. Annals of the New York Academy of Sciences, 966, 131–142. https://doi.org/10.1111/j.1749-6632.2002.tb04210.x
- Gooch, J. W. (2011). Nonspecific Defenses. In Encyclopedic Dictionary of Polymers (pp. 910–910). Springer New York. https://doi.org/10.1007/978-1-4419-6247-8_14340
- Klein, S. L. (2012). Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. BioEssays, 34(12), 1050–1059. https://doi.org/10.1002/bies.201200099
- Nakashima, A., Ohkido, I., Yokoyama, K., Mafune, A., Urashima, M., & Yokoo, T. (2017). Associations Between Low Serum Testosterone and All-Cause Mortality and Infection-Related Hospitalization in Male Hemodialysis Patients: A Prospective Cohort Study. Kidney International Reports, 2(6), 1160–1168. https://doi.org/10.1016/j.ekir.2017.07.015
- Robinson, D. P., Hall, O. J., Nilles, T. L., Bream, J. H., & Klein, S. L. (2014). 17 -Estradiol Protects Females against Influenza by Recruiting Neutrophils and Increasing Virus-Specific CD8 T Cell Responses in the Lungs. Journal of Virology, 88(9), 4711–4720. https://doi.org/10.1128/jvi.02081-13
- Tatiana, Z. (2012). Gonadal Sex Steroids: Production, Action and Interactions in Mammals. In Steroids – From Physiology to Clinical Medicine. InTech. https://doi.org/10.5772/52994
- Trumble, B. C., Blackwell, A. D., Stieglitz, J., Thompson, M. E., Suarez, I. M., Kaplan, H., & Gurven, M. (2016). Associations between male testosterone and immune function in a pathogenically stressed forager-horticultural population. American Journal of Physical Anthropology, 161(3), 494–505. https://doi.org/10.1002/ajpa.23054
- (2020). Leishmaniasis. https://www.who.int/en/news-room/fact-sheets/detail/leishmaniasis